Impotence or Erectile Dysfunction (ED) is the persistent inability to maintain a penile erection long enough for satisfactory sexual activity. It is a common problem in men with Type 2 Diabetes Mellitus, with studies showing that 50% to 75% of adult men are affected. This early onset of Impotence in diabetes often signals underlying health complications that require timely attention.
Treating ED with diabetes depends mainly on oral ED medicines known as Phosphodiesterase type 5 (PDE5) inhibitors. These Safe ED pills form the first-line therapy when there are no contraindications. Men with diabetes often need higher doses of these medications to achieve results. A Prescription is always required after a medical assessment to ensure proper use. Other options for ED treatment for diabetics include testosterone replacement in men with hypogonadism, vacuum constriction devices, and intracavernosal injections.
Natural remedies for ED play a strong role in improving sexual health among diabetic patients. Lifestyle changes such as increasing physical activity, reducing weight, and stopping smoking can support erection quality and overall health. These methods act as supportive therapy along with prescribed treatment.
Prevention of Impotence in diabetes depends on good control of blood glucose. According to a study titled “Study of erectile dysfunction in patients of type 2 diabetes mellitus and its association with cardiovascular risk”, poor glycemic control is a significant risk factor for ED in diabetic men. This shows that strict management of blood sugar levels is critical to prevent the early development of ED.
Medical consultation is necessary for men with diabetes who experience persistent erection problems. All men with diabetes should undergo regular screening for ED by reporting their sexual health history. When PDE5 inhibitors do not work or when they are not safe to use, patients require referral to a specialist for advanced ED treatment. The safest way to access effective medicines is through a doctor’s prescription and licensed sources that provide Safe ED pills.
What is Impotence or ED?
Impotence or Erectile Dysfunction (ED) is the inability to sustain an adequate penile erection for satisfactory sexual activity. According to a study titled “Study of erectile dysfunction in patients of type 2 diabetes mellitus and its association with cardiovascular risk,” ED is the persistent inability to achieve and maintain penile erection sufficient for adequate sexual intercourse for at least 6 months. ED is a common medical disorder that negatively impacts the quality of life in men.
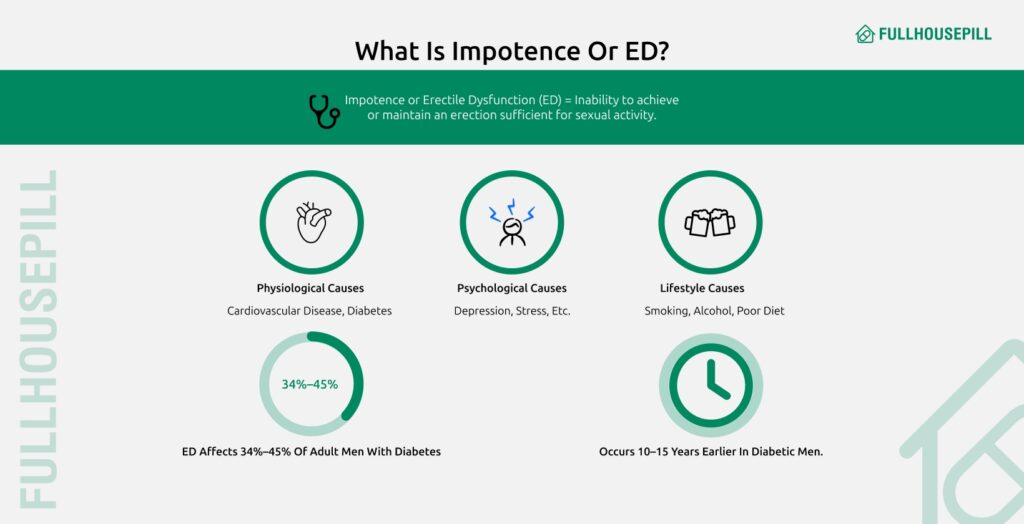
Occasional issues with erection may result from stress or tiredness. However, ongoing problems with ED can signal serious health issues, including heart disease or diabetes. ED often stems from multiple factors, including physiological, psychological, and lifestyle elements. According to chapter 29, Male sexual dysfunction in type 2 diabetes, South African Family Practice, depression affects 28% of men with Type 2 Diabetes Mellitus (T2DM), while up to 20% of ED cases result from psychogenic causes.
Modifiable risk factors for ED include smoking, lack of physical activity, poor diet, obesity, metabolic syndrome, and excessive alcohol consumption. These conditions create a pro-inflammatory state that reduces nitric oxide availability and causes endothelial dysfunction. Ongoing ED problems serve as early clinical indicators of cardiovascular disease (CVD) and other serious health conditions, including coronary artery disease (CAD).
ED is treatable through lifestyle changes, medication, or other interventions. Consulting a doctor is crucial for proper diagnosis and treatment. All adult men with diabetes should receive regular ED screening using a sexual function history. Treatment includes lifestyle modifications such as increasing physical exercise, reducing weight by 5-10%, and stopping smoking. PDE5 inhibitors serve as first-line therapy for men with diabetes without hypogonadism.
ED affects approximately 34% to 45% of adult men with diabetes. According to a systematic review titled “Phosphodiesterase-5 inhibitors for erectile dysfunction in patients with diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials,” the prevalence ranges from 35% to 90% in diabetic patients. ED in diabetic men occurs 10-15 years earlier, tends to be more severe, and responds less to oral drugs compared to men without diabetes. Poor glycemic control serves as a major risk factor for ED, while better glycemic control reduces peripheral neuropathy and maintains erectile function.
Can Diabetes Cause Impotence or Erectile Dysfunction?
Yes, diabetes can cause erectile dysfunction (ED). Diabetes damages blood vessels and nerves essential for an erection. High blood sugar damages nerves and blood vessels needed for an erection through multiple mechanisms. Diabetes causes micro and macrovascular complications that contribute to ED. Diabetes also causes peripheral neuropathy, which impairs sensory feedback from the penis resulting in erectile dysfunction. Both Type 1 and Type 2 diabetes affect ED. According to Chapter 29 in the journal South African Family Practice,” 50% to 75% of adult men with Type 2 diabetes experience ED. One-third of newly diagnosed diabetic men have ED at presentation. ED is often treatable with diabetes. According to clinical practice guidelines titled “Sexual Dysfunction and Hypogonadism in Men With Diabetes,” PDE5 inhibitors serve as the current mainstay therapy for ED in diabetic men. Treatment combines lifestyle modifications with medication. Optimal glycemic control serves as a potential factor in maintaining erectile function.
How Does Type 1 Diabetes Cause ED?
The ways Type 1 diabetes can cause ED are listed below.
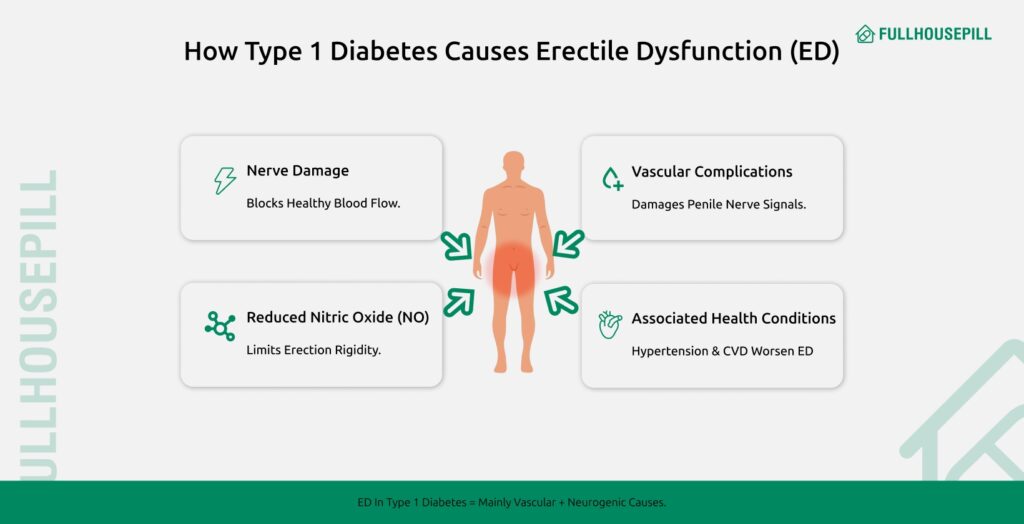
- Damage to Nerves (Peripheral Neuropathy): Poor glycemic control damages nerves carrying essential sensory feedback from the penis. According to a journal titled “South African Family Practice,” better glycemic control leads to reductions in peripheral neuropathy.
- Vascular/Microvascular Complications: Type 1 diabetes frequently causes micro and macrovascular complications, impairing endothelial function necessary for normal erection. According to a study titled “Intracavernosal alprostadil is effective for the treatment of erectile dysfunction in diabetic men,” vascular and neurogenic complications are the main causes of ED in diabetic men.
- Reduced Nitric Oxide (NO) Availability: Diabetes causes endothelial dysfunction, reducing nitric oxide availability crucial for increasing genital blood flow required for rigidity. According to a study titled “Lifestyle modifications and erectile dysfunction: what can be expected?” nitric oxide serves as the driving force of genital blood flow.
- Associated Health Conditions: Risk factors, including increasing age, poor glycemic control, hypertension, and cardiovascular disease commonly seen in diabetes, contribute to ED. According to clinical practice guidelines titled “Sexual Dysfunction and Hypogonadism in Men With Diabetes,” ED can serve as an early sign of cardiovascular disease in Type 1 diabetes.
The overall pathology for diabetes-related ED in Type 1 diabetes involves these vascular and neurogenic pathways. A study titled Intracavernosal alprostadil is effective for the treatment of erectile dysfunction in diabetic men notes that microangiopathy is often more pronounced in Type 1 diabetes, which can reduce the effectiveness of intracavernosal vasoactive therapy. While these mechanisms dominate in Type 1 diabetes, Type 2 diabetes introduces additional hormonal, metabolic, and psychological factors that further complicate erectile function.
How Does Type 2 Diabetes Cause ED?
The ways Type 2 diabetes can cause ED are listed below.
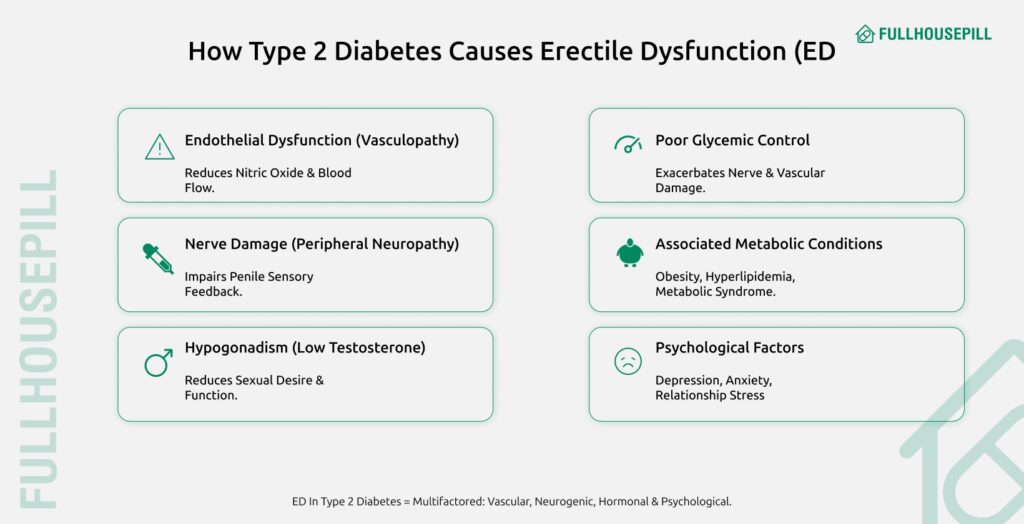
- Endothelial Dysfunction (Vasculopathy): Endothelial damage in T2DM reduces nitric oxide needed for erection. According to chapter 29, Male sexual dysfunction in type 2 diabetes, in South African Family Practice,” endothelial dysfunction explains the consistent association between ED and cardiovascular risk.
- Nerve Damage (Peripheral Neuropathy): Poor glycemic control damages peripheral nerves, impairing sensory feedback needed to initiate an erection. According to a chapter titled “Male sexual dysfunction in type 2 diabetes” in South African Family Practice, peripheral neuropathy results in ED.
- Hypogonadism (Low Testosterone): T2DM increases the risk of hypogonadotropic hypogonadism, reducing sexual desire and affecting erectile function. According to clinical practice guidelines titled “Sexual Dysfunction and Hypogonadism in Men With Diabetes,” low testosterone is common in men with Type 2 diabetes.
- Poor Glycemic Control: High fasting and postprandial blood glucose levels exacerbate vascular and nerve damage, directly contributing to ED. According to a study titled “Study of erectile dysfunction in patients of type 2 diabetes mellitus and its association with cardiovascular risk,” poor glycemic control is the strongest risk factor for ED.
- Associated Metabolic Conditions: Obesity, hyperlipidemia, and metabolic syndrome create a pro-inflammatory state, reducing nitric oxide and impairing blood flow. According to a study titled “Lifestyle modifications and erectile dysfunction: what can be expected?” these conditions lead to endothelial dysfunction.
- Psychological Factors: Depression, performance anxiety, and relationship issues common in T2DM significantly contribute to ED severity. According to a journal titled “South African Family Practice,” depression was present in 28% of men with T2DM.
What are The Early Signs of ED in Diabetics?
The early signs of ED in diabetics include difficulty achieving or maintaining a penile erection for sexual activity. The first noticeable symptom is reduced penile rigidity during intercourse. This problem often occurs 10–15 years earlier in men with diabetes compared to non-diabetics. However, up to one-third of newly diagnosed diabetic men experience ED, making it an early marker of other health issues.
ED in diabetes may appear with symptoms of hypogonadism. These include low sexual desire, reduced libido, and loss of nocturnal erections. Low testosterone, common in men with Type 2 diabetes, is often responsible for these changes. High blood sugar damages blood vessels and nerves. This damage impairs endothelial function and lowers nitric oxide availability, which is essential for blood flow to the penis. Reduced nitric oxide makes it difficult to achieve a normal erection. Poor glycemic control also causes peripheral neuropathy, which blocks sensory signals from the penis and worsens erectile problems.
Other health risks in diabetes make ED more severe. Hypertension, dyslipidemia, and chronic inflammation increase vascular and nerve injury. These risk factors link ED to cardiovascular disease and higher mortality rates. Psychological symptoms often appear alongside physical ones. Depression, anxiety, and performance pressure can worsen erectile dysfunction. A meta-analysis titled, “The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies”, reports that depression affects about 28% of men with Type 2 diabetes.
Recognizing erectile dysfunction (ED) early in patients with diabetes is crucial. Doctors recommend screening for sexual dysfunction at the time of diabetes diagnosis. Early intervention with lifestyle changes and first-line therapy like PDE5 inhibitors can improve erectile function. These treatments also help reduce cardiovascular risk and improve overall health.
How to Treat Impotence or Erectile Dysfunction in Diabetes?
Treating impotence or Erectile Dysfunction includes a comprehensive strategy combining lifestyle management, pharmacological interventions, device therapies, hormonal treatment, and psychological support. Treatment options for impotence or Erectile Dysfunction are listed below.
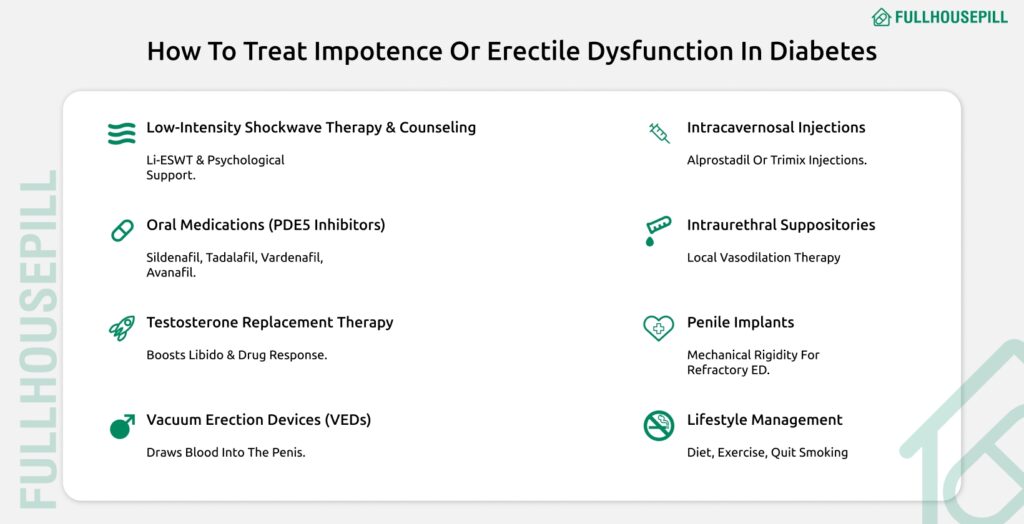
- Manage diabetes with lifestyle changes: Modifying diet, exercise, and smoking habits reduces inflammation and improves endothelial function by increasing nitric oxide availability.
- Oral medications (PDE5 inhibitors): Oral ED meds such as sildenafil for diabetics, tadalafil for diabetics, vardenafil for diabetics, and avanafil for diabetics inhibit phosphodiesterase type 5 to increase cGMP and promote vasodilation.
- Testosterone replacement therapy: Administering testosterone to hypogonadal men with diabetes improves libido and augments PDE5 response.
- Vacuum erection devices: VEDs create negative pressure to draw blood into the penis, maintained by a constriction band.
- Intracavernosal injections: Alprostadil or trimix injections directly dilate penile arteries for rapid erection.
- Intraurethral suppositories: Urethral pellets of alprostadil induce localized vasodilation as second-line therapy.
- Penile implants: Surgical insertion of a penile prosthesis provides mechanical rigidity when all other treatments fail.
- Low-intensity shockwave therapy: Li-ESWT applies shockwaves to penile tissue to stimulate neovascularization in refractory cases.
- Counselling or sex therapy: Psychological and emotional support addresses depression, performance anxiety, and relationship factors.
- Manage diabetes with lifestyle changes
Lifestyle changes involve modifying behaviors associated with ED risk, such as changing diets, increasing physical activity, stopping smoking, managing weight (overweight or obesity), and moderating alcohol consumption. Healthy lifestyles are key factors influencing vascular nitric oxide (NO) production and erectile function. NO is the driving force of genital blood flow.
Lifestyle changes are believed to reduce low-grade clinical inflammation, which consequently improves endothelial function. Physical activity enhances cardiovascular fitness, increases endothelial-derived NO, and reduces oxidative stress. Weight loss, whether achieved by lifestyle or bariatric intervention, is linked to a rise in testosterone and a decline in estrogen levels. Improving glycaemic control is advised as a potential factor for maintaining erectile function in individuals with diabetes. The European Association of Urology determined that lifestyle changes and risk factor modification must precede or accompany ED treatment, classifying this intervention with Level of Evidence 1b and Grade A
According to a meta-analysis, engaging in moderate to high levels of physical activity is linked to a reduced risk of erectile dysfunction (ED), with odds ratios of 0.63 and 0.42, respectively. A randomized controlled trial titled “Effect of Lifestyle Changes on Erectile Dysfunction in Obese Men” found that participants who underwent intensive lifestyle changes experienced greater weight loss, increased physical activity, and significant improvements in their ED scores compared to the control group after two years.
In the Look AHEAD trial, only 8% of men assigned to an intensive lifestyle intervention reported a worsening of erectile function, compared to 22% of those in the control group. This resulted in an overall improvement in the International Index of Erectile Function (IIEF) scores for the intervention group.
Another study, titled “Mediterranean Diet Improves Erectile Function in Subjects with the Metabolic Syndrome,” involved 65 men with metabolic syndrome and ED. After two years, those adhering to the Mediterranean diet showed improvements, with 13 men in the intervention group increasing their IIEF scores by up to 22, while only 2 men in the control group showed similar progress.
Additionally, a review in the Asian Journal of Andrology found that a 10% weight loss in diabetic men was associated with increased insulin sensitivity, higher plasma testosterone levels, and improved IIEF-5 scores. Overall, lifestyle modifications are a highly effective approach for both the prevention and treatment of ED, offering benefits for overall health and reducing the impact of sexual dysfunction.
- Oral medications (e.g., sildenafil, tadalafil, vardenafil, avanafil)
These are Oral ED meds, classified as Phosphodiesterase type 5 (PDE5) inhibitors. They are the mainstay and cornerstone of therapy for ED and are recommended as first-line treatment for men with diabetes, provided they have no contraindications. PDE5 inhibitors prevent the metabolism of Cyclic guanosine monophosphate (cGMP) in the corpus cavernosum. Upon sexual stimulation, nitric oxide is released, increasing cGMP levels. By inhibiting the breakdown of cGMP, PDE5 inhibitors sustain vasodilation and increased blood flow to the penis, thus enabling an erection.
A systematic review and meta-analysis titled “Phosphodiesterase-5 inhibitors for erectile dysfunction in patients with diabetes mellitus” concluded that PDE5 inhibitors are effective and safe for ED in patients with diabetes mellitus. The pooled mean effect size for any PDE5 inhibitor over placebo was 0.926. The overall Number Needed to Treat (NNT) for all PDE5 inhibitors combined was 3.0. Men with diabetes often require a higher dose of the PDE5 inhibitor, and about 50% usually respond adequately to therapy. The pooled mean effect size for Sildenafil for diabetics against placebo was 1.198, which was the highest among the specific drugs analyzed. The NNT for sildenafil was 2.4. A randomized controlled trial titled “Sildenafil for treatment of erectile dysfunction in men with diabetes” evaluated sildenafil in this population. The pooled mean effect size for Tadalafil for diabetics against placebo was 0.910. The NNT for tadalafil was 2.6. The SURE study evaluated the efficacy and safety of two dosing regimens of tadalafil in men with diabetes. The pooled mean effect size for Vardenafil for diabetics against placebo was 0.678. The NNT for vardenafil was 4.1. A multicentre study titled “Vardenafil, a new phosphodiesterase type 5 inhibitor, in the treatment of erectile dysfunction in men with diabetes” demonstrated its use in diabetic men. The effect sizes for Avanafil for diabetics (100 mg and 200 mg) compared to placebo were 0.391 and 0.524, respectively, according to the study by Goldstein et al.. The NNT for Avanafil 100 mg was 7.2.
PDE5 inhibitors are strictly contraindicated with concurrent nitrate use. They are considered safe for men with stable ischemic heart disease who do not use nitrates. The most common adverse events include headache, dyspepsia, hot flushes/flushing, rhinitis, and nasal congestion. Adverse events for the active PDE5 drug were approximately twice as common as with placebo.
- Testosterone replacement therapy
Testosterone Replacement Therapy (TRT) is a treatment approved for hypogonadism, a condition common in men with type 2 diabetes (up to 40% prevalence). TRT aims to restore testosterone levels to the normal range. Testosterone regulates nearly every aspect of erectile function, including the timing of the erectile process. Testosterone Therapy (TTh) can improve libido, vigor, depressed mood, muscle strength, and insulin sensitivity. Treatment of hypogonadism before initiating PDE5 inhibitor therapy reduces the number of non-responders.
A systematic review and meta-analysis titled “Treatment with Testosterone Therapy in Type 2 Diabetic Hypogonadal Adult Males” found that TRT significantly improved post-treatment glycated hemoglobin (HBA1c) levels. This study also showed that TRT is associated with a significant increase in total testosterone levels. The analysis suggests that TRT can lower total cholesterol, triglycerides, and LDL cholesterol while raising HDL cholesterol, in addition to improving glycemic control and hormone levels. A prospective observational study showed that hypogonadal obese men with Type 2 diabetes who were treated with testosterone lost weight and showed improvement in cardiovascular risk factors.
Monitoring after TTh initiation includes assessing symptom resolution, side effects, serum testosterone, Prostate Specific Antigen (PSA), haematocrit, and regular Digital Rectal Examination (DRE). Polycythemia (haematocrit levels above 54%) is a risk that may necessitate therapeutic phlebotomy or discontinuation of TTh. Recent evidence does not support the concern of a link between prostate cancer and TTh or that TTh promotes subclinical prostatic lesion growth. However, prostate assessment (PSA and DRE) is still recommended prior to TTh commencement. Observational studies on the impact of testosterone use on cardiovascular health have produced conflicting results.
- Vacuum erection devices
These are mechanical devices, also known as vacuum constriction devices or vacuum tumescence therapy. They are considered a second-line therapy for ED, usually for patients who fail to respond to PDE5 inhibitors. The device creates a vacuum effect around the penis, drawing blood into the corpora cavernosa to achieve rigidity adequate for sexual intercourse. A constriction ring is then placed at the base of the penis to maintain the erection.
A study titled “The management of impotence in diabetic men by vacuum tumescence therapy” investigated its use in diabetic men with impotence. Of 44 diabetic men who chose vacuum therapy, 33 men (75%) were able to achieve satisfactory intercourse after 2 months. The study found that the outcome was independent of factors such as penile blood flow or endocrine status. Vacuum erection devices may also be used in combination with PDE5 inhibitors as salvage therapy for non-responders.
Treatment is generally simple and effective. In the mentioned study, a risk factor was partner acceptability, as three men who achieved satisfactory erections found their partners rejected the treatment.
- Intracavernosal injections (e.g., alprostadil, trimix)
These are second-line treatments for ED, typically recommended if PDE5 inhibitors are contraindicated or fail. They involve injecting vasoactive agents directly into the corpora cavernosa. Agents include alprostadil (prostaglandin E1 or PGE1) alone, or in combinations like trimix (PGE1 with papaverine and phentolamine). Intracavernosal alprostadil (PGE1) is a vasoactive substance that causes vasodilation when injected, increasing blood flow to the penis to facilitate an erection.
According to the study “Intracavernosal alprostadil is effective for the treatment of erectile dysfunction in diabetic men,” alprostadil was effective and well-tolerated in Type I and Type II diabetic men. An effective home dose was established by titration for 94% of the 336 men enrolled. During the 6-month home phase, a satisfactory erectile response was reported after 99% of injections. Response rates were similar in Type I and Type II diabetic men.
Treatment is generally well tolerated, but safety depends on careful dose titration. The adverse event profile is consistent with previous reports. The incidence of penile pain was 24%. Other risks included prolonged erection or priapism (>6 hours), which occurred in 1% of patients but resolved spontaneously. Treatment discontinuation occurred in 5% of men, primarily due to penile pain.
- Intraurethral suppositories
This is a second-line therapy for ED, involving the administration of medication, typically prostaglandin E1 (PGE1), via a suppository inserted into the urethra. The vasoactive agent (PGE1) is absorbed through the urethra to induce a therapeutic erection. Intraurethral therapy using PGE1 is listed as a second-line therapy option for men who do not respond to PDE5 inhibitors or have contraindications, requiring referral to an ED specialist.
- Penile implants
These are penile prostheses, constituting a third-line therapy for ED. Penile implants are surgical devices used to correct erect penile deformity in men with stable disease, such as Peyronie’s disease. They provide a mechanical means to achieve rigidity for sexual activity. They are considered when second-line therapies (like vacuum devices or injections) fail. A study mentions the efficacy, safety, and patient satisfaction outcomes of the AMS 700CX inflatable penile prosthesis. Penile implants are a surgical option; specific safety details for diabetic men are not detailed in the sources, other than their designation as a third-line therapy.
- Low-intensity shockwave therapy
Low-Intensity Shockwave Therapy (Li-ESWT) is an evidence-based, non-invasive treatment for Erectile Dysfunction (ED) in men with diabetes mellitus. The therapy uses acoustic waves to stimulate cellular pathways, enhancing endothelial function, angiogenesis, and nerve regeneration. It effectively improves penile blood flow and can convert PDE5 inhibitor non-responders into responders.
Li-ESWT activates local growth factors, improves vascular health, and promotes new blood vessel formation for stronger erections. It may also support nerve repair in diabetic patients with vascular or neuropathic ED. A Clinical study in the “African Journal of Urology” reports significant improvements in International Index of Erectile Function (IIEF) scores, showing long-term gains in erectile function. The treatment is safe, painless, and drug-free, with no major side effects.
During each session, an ultrasound gel and shockwave probe deliver controlled acoustic pulses, producing a mild tapping sensation. Combining Li-ESWT with daily tadalafil may further enhance and sustain results. Li-ESWT offers diabetic men a clinically proven, well-tolerated, and long-lasting solution for erectile dysfunction.
- Counselling or Sex therapy
This involves psycho-sexual intervention, encompassing Counselling or Sex therapy (cognitive/behavioural therapy). This includes the provision of Emotional support. This modality addresses Psychological factors, such as depression, performance anxiety, and relationship issues, which significantly contribute to ED. Psychological factors are one of the multiple causes of ED in Type 2 diabetes. Furthermore, physical activity itself positively impacts Psychological issues like self-esteem and mental health, often associated with sexual dysfunction. Addressing these issues is part of the comprehensive evaluation and treatment of sexual dysfunction.
According to a large meta-analysis of 51,331 patients, depression was present in 28% of men with T2DM. A further review highlights that ED is strongly linked with anxiety and depression, noting that up to 20% of ED cases are attributed to a psychogenic cause. Emotional support and addressing relationship dissatisfaction are crucial components of ED management in diabetic men. This approach is recommended as part of concurrent treatment alongside medical interventions and lifestyle modification.
Can Diabetes Medication Worsen ED?
Yes, diabetes medications can worsen ED by affecting testosterone levels, libido, and blood vessel and nerve health. Certain drugs negatively influence endocrine status, amplifying hypogonadism and reducing sexual desire. Some cardiovascular and neuropathic pain medications impair endothelial function and neural pathways essential for erection. Antihypertensives such as β-blockers and thiazide diuretics have been linked to ED in diabetic men, according to a study titled “Study of erectile dysfunction in patients of type 2 diabetes mellitus and its association with cardiovascular risk”.
Antidepressants commonly prescribed for depression also contribute to ED. Lipid-lowering agents like statins and fibrates are associated with ED in the same study. Metformin use has been linked to ED, and some trials exclude sulfonylureas or ACE inhibitors for their potential impact on erectile function. Drugs for neuropathic pain, such as pregabalin and gabapentin, further increase the risk of nerve damage and ED. Uncontrolled diabetes itself remains a major cause of ED. Identifying reversible medication-related causes is crucial, and clinicians should review drug history before prescribing treatments like testosterone.
Treating erectile dysfunction with lifestyle modifications is an important approach. First-line approaches combine glycemic control with exercise, weight loss, smoking cessation, and dietary improvements. These methods aim to reduce inflammation, enhance nitric oxide availability, and improve erectile function. Consulting a healthcare provider ensures safe adjustment of medications and optimal ED management.
What are The Natural Remedies for ED in Diabetes Patients?
Treating ED naturally in diabetes patients involves intensive lifestyle and dietary strategies that improve vascular health, glycemic control, and psychological well-being. Natural remedies for ED in diabetes patients are listed below.
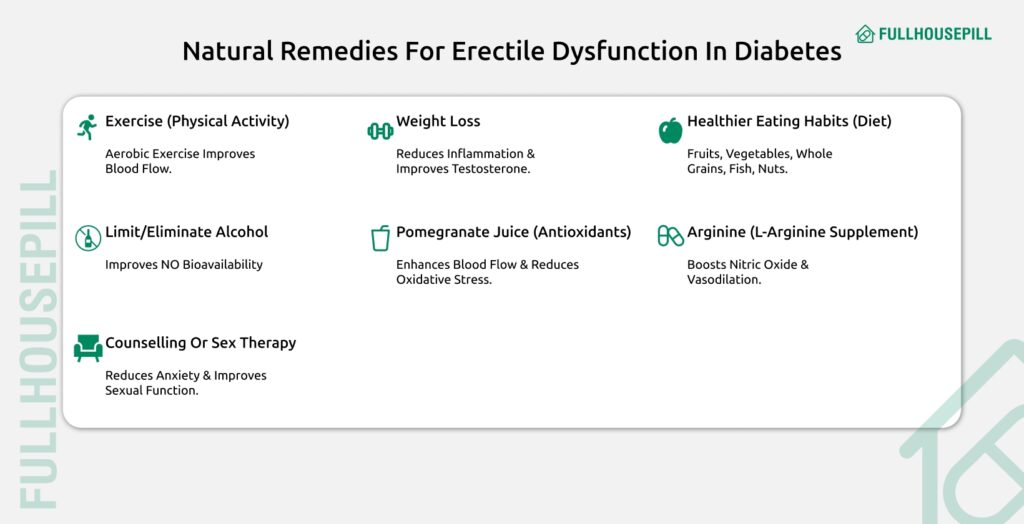
- Exercising (Physical Activity): Regular aerobic exercise improves endothelial function, raises nitric oxide, and reduces oxidative stress. A study titled “Lifestyle modifications and erectile dysfunction: what can be expected?” showed 77.8% ED restoration with ≥3 hours/week exercise plus PDE5 inhibitors versus 39.3% without.
- Lose Weight (Weight Loss): Reducing body weight by 5%–10% lowers inflammation, improves insulin sensitivity, and raises testosterone. Trials in “Lifestyle modifications and erectile dysfunction: what can be expected?” demonstrated ED improvement or resolution in obese patients.
- Healthier Eating Habits (Dietary Factors): A Mediterranean-style diet rich in fruits, vegetables, whole grains, nuts, and fish reduces inflammation and enhances NO release. In “Adherence to Mediterranean diet and erectile dysfunction in men with type 2 diabetes,” greater adherence correlated with lower ED prevalence.
- Limit or Eliminate Alcohol (Moderate Consumption/Cessation): Moderate alcohol (1–20 drinks/week) improves HDL and NO bioavailability, lowering ED risk. According to “Lifestyle modifications and erectile dysfunction: what can be expected?”, ED odds were lowest among moderate drinkers.
- Pomegranate Juice (Dietary Antioxidants): Pomegranate extract improves intracavernosal blood flow, smooth-muscle relaxation, and erectile activity by reducing oxidative products. A rabbit atherosclerosis model in “Lifestyle modifications and erectile dysfunction: what can be expected?” confirmed these benefits.
- Arginine (L-Arginine Supplementation): L-Arginine provides a substrate for NO synthesis, enhancing vasodilation. Arginine’s combination with PDE5 inhibitors shows synergistic effects in trials cited in “Phosphodiesterase-5 inhibitors for erectile dysfunction in patients with diabetes mellitus”.
- Counselling or Sex Therapy: Addressing depression, performance anxiety, and relationship issues provides emotional support and improves sexual function.
Can Lifestyle Changes and Self-Care Help with ED?
Yes, lifestyle changes and self-care can help with ED by improving vascular health, reducing inflammation, and optimizing metabolic control. Lifestyle changes and self-care in ED management include physical activity, weight reduction, smoking cessation, and dietary improvements, especially reducing sugar. Increasing physical exercise improves cardiovascular fitness, raises endothelial-derived nitric oxide, and reduces oxidative stress. A meta-analysis titled “Physical activity and erectile dysfunction: meta-analysis of population-based studies” found that moderate to high activity lowers ED risk.
Reduce weight by 5%–10% or achieve a BMI ≤30 kg/m² to decrease visceral fat, improve insulin sensitivity, and raise testosterone. An RCT in “Effects of a low-energy diet on sexual function and lower urinary tract symptoms in obese men” linked 10% weight loss to improved IIEF-5 scores. Smoking cessation restores endothelial function by eliminating tobacco-induced vascular damage. The study “Association between smoking cessation and sexual health in men” reported significant improvements in physiological and self-reported sexual health after quitting.
Adopt healthier eating habits by reducing added sugars and refined grains and following a Mediterranean-style diet rich in whole grains, fruits, vegetables, and nuts. According to “Adherence to Mediterranean diet and erectile dysfunction in men with type 2 diabetes,” greater diet adherence was associated with lower ED prevalence.
Does Sugar Increase the Chance of Erectile Dysfunction?
Yes, sugar does increase the chance of Erectile Dysfunction because high blood glucose levels damage both the neurological and vascular systems essential for an erection. According to the study titled “Study of erectile dysfunction in patients of type 2 diabetes mellitus and its association with cardiovascular risk,” poor glycemic control emerged as the strongest risk factor for ED. That study also found that patients with ED had significantly higher mean values of fasting blood sugar (FBS) and postprandial blood sugar (PPBS), with correlations reaching statistical significance (p < 0.05).
High glucose levels lead to microvascular and macrovascular complications that undermine erectile function. Chronic hyperglycemia causes endothelial dysfunction by reducing the availability and activity of nitric oxide, the molecule that drives genital blood flow. Prolonged elevated blood sugar further contributes to peripheral neuropathy, impairing the sensory feedback from the penis and leading to erectile difficulties. Data from the Diabetes Control and Complications Trial and the United Kingdom Prospective Diabetes Study demonstrate that tighter glycemic control reduces the incidence and progression of peripheral neuropathy. Since neuropathy is an organic cause of ED, these findings underscore the benefit of managing sugar intake and blood glucose to preserve erectile function.
Prevention of ED through lifestyle modification and rigorous self-care is vital, particularly for men with diabetes. Erectile dysfunction often presents 10–15 years earlier in diabetic men and can serve as an early clinical warning of cardiovascular disease. Addressing elevated sugar levels not only helps maintain erectile function but also reduces overall cardiovascular risk. According to the article “Lifestyle modifications and erectile dysfunction: what can be expected?” guidelines from the European Association of Urology recommend that dietary improvements, increased physical activity, weight reduction, and strict glycemic control should precede or accompany ED treatment for optimal outcomes.
How to Prevent ED in Diabetics?
Preventing erectile dysfunction in men with diabetes relies on strict blood sugar control, cardiovascular risk management, and healthy lifestyle habits. This approach combines medical screening with self-care measures to protect nerve and blood vessel health.

- Achieving Optimal Glycemic Control
Maintaining blood glucose levels within target ranges, focusing on reducing sustained hyperglycemia reflected by measures like HbA1c, FBS, and PPBS. Improved glycaemic control reduces the incidence and progression of peripheral neuropathy, which impairs sensory feedback necessary for erection, thus helping maintain erectile function.
- Regular Physical Exercise
Engaging in structured physical activity, such as regular aerobic exercise, typically involves accumulating 150 minutes per week. Exercise improves endothelial function, enhances nitric oxide (NO) bioavailability, reduces oxidative stress, and is generally associated with a lower risk of ED.
- Smoking Cessation
Smoking is a consolidated risk factor for ED because it causes vascular and endothelial damage; quitting reverses these negative effects on sexual health indices.
- Weight Reduction and Management
Reducing weight, particularly abdominal/visceral fat, aiming for a loss of 5–10% or maintaining a body mass index (BMI)≤30 kg/m². Weight loss targets metabolic syndrome and the associated pro-inflammatory state, improving endothelial function, insulin sensitivity, and naturally increasing testosterone levels.
- Adopting a Healthy Diet
Consuming diets rich in vegetables, fruits, whole grains, and fish, and limiting red meat and foods high in added sugars. Healthy diets, such as the Mediterranean diet, reduce inflammation and oxidative stress, thereby improving endothelial function and NO release in penile arteries.
- Screening and Management of Comorbidities
Regularly screening for and treating associated risk factors like hypertension, dyslipidemia, depression, and hypogonadism. ED is strongly associated with CVD risk factors; managing these comorbidities (e.g., controlling blood pressure and cholesterol) reduces generalized vascular damage common to both ED and heart disease.
- Counselling and Psychological Support
Utilizing counseling, behavioral therapy, or sex therapy to address psychological and relationship issues. This addresses factors like performance anxiety and depression, which commonly contribute to ED in diabetic men, ensuring a holistic approach to sexual well-being.
Should Diabetic People Have Sex?
Yes, diabetic people should engage in sexual activity if they wish, as fulfilling sexual health supports overall quality of life. Diabetes can cause erectile dysfunction in men and vaginal dryness or decreased libido in women through vascular, neurological, and hormonal pathways. According to a study titled “Phosphodiesterase-5 inhibitors for erectile dysfunction in patients with diabetes mellitus,” sexual dysfunction in diabetic men is linked to poor quality of life and marital dissatisfaction. Men with diabetes may also experience ejaculatory disorders and low testosterone, while women can develop arousal disorders responsive to PDE5 inhibitors.
To reduce risks, diabetic individuals should monitor blood glucose before and during sex, keep fast-acting carbohydrates nearby to prevent hypoglycemia, and review medications that affect circulation or interact with sexual function. Discussing these precautions with a doctor can help tailor a safe plan. Consulting a healthcare expert is essential. The guidelines titled “Sexual Dysfunction and Hypogonadism in Men With Diabetes – Clinical Practice Guidelines” recommend screening all men with Type 2 diabetes for sexual dysfunction at diagnosis and crafting personalized strategies that address glycemic control, comorbidities, and psychological factors.
When to See a Doctor for Impotence in Diabetics?
A person should see a doctor for impotence in diabetes if they experience persistent difficulty achieving or maintaining an erection, as this may signal poorly controlled diabetes, heart disease, or other serious issues. According to “Sexual Dysfunction and Hypogonadism in Men With Diabetes – Clinical Practice Guidelines,” all adult men with diabetes require regular ED screening starting at diagnosis. When erectile problems indicate poor glycemic control, a doctor can adjust diabetes management; the study titled “Study of erectile dysfunction in patients of type 2 diabetes mellitus and its association with cardiovascular risk” found poor glycemic control to be the strongest ED risk factor. Since ED can be an early marker of cardiovascular disease, a medical evaluation can assess heart risk. Before taking any medication like sildenafil (Viagra), one must consult a doctor to avoid contraindications such as concurrent nitrate use and to ensure proper diagnosis and treatment planning.
Can Men with Type 2 Diabetes Take Sildenafil?
Yes, men with Type 2 diabetes can take Sildenafil tablets because Phosphodiesterase type 5 (PDE5) inhibitors are the first-line therapy for diabetic erectile dysfunction. Sildenafil works by blocking PDE5, which prolongs cyclic guanosine monophosphate (cGMP) action in the corpus cavernosum. This enhances nitric oxide–mediated vasodilation and increases penile blood flow, helping initiate and maintain an erection. According to a systematic review and meta-analysis titled “Phosphodiesterase-5 inhibitors for erectile dysfunction in patients with diabetes mellitus,” sildenafil showed a pooled effect size of 1.198 and an NNT of 2.4, making it both effective and safe in diabetic men. Before starting Sildenafil, consulting a doctor is essential to evaluate contraindications, especially concurrent nitrate use. It is important to assess hypogonadism and review potential drug interactions. Additionally, a doctor can determine the optimal dosing regimen.
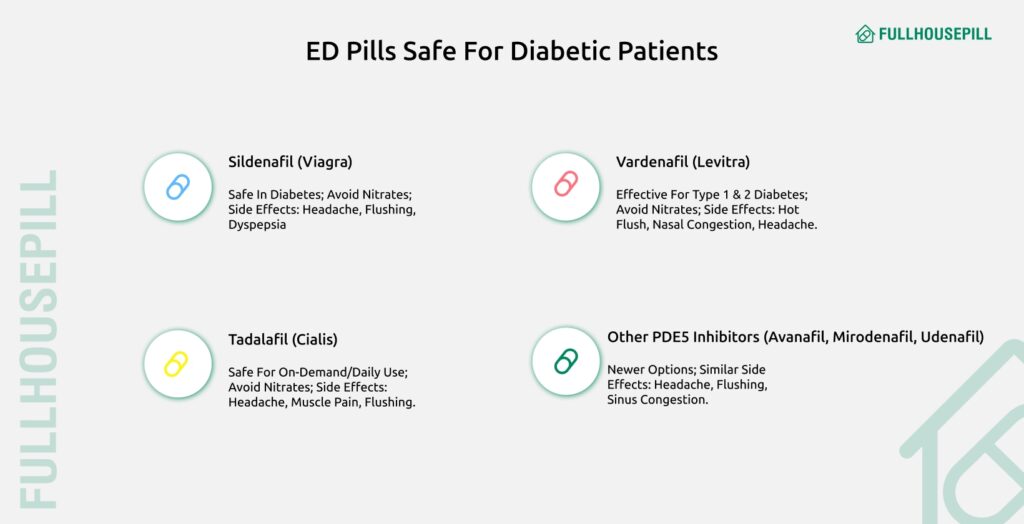
What ED Pills are Safe for Diabetics?
The safety and efficacy of ED pills for diabetic patients largely rely on a class of drugs known as Phosphodiesterase Type 5 (PDE5) inhibitors, which are generally recommended as first-line therapy. Treatment options for impotence or Erectile Dysfunction are listed below.
- Sildenafil (Viagra):
It is an oral PDE5 inhibitor that has been widely evaluated in randomized controlled trials (RCTs) for treating ED in diabetic men. Sildenafil is generally effective and safe, but it is absolutely contraindicated with concurrent nitrate use. Common adverse events include headache, dyspepsia, and flushing, but diabetics may have lower rates of side effects.
- Tadalafil (Cialis):
Tadalafil is an oral PDE5 inhibitor used for ED treatment, evaluated in clinical trials for both on-demand and scheduled daily use in diabetic men. Tadalafil is considered effective and safe. It is absolutely contraindicated with concurrent nitrate use. Common adverse events include headache, dyspepsia, flushing, and myalgia (muscle pain).
- Vardenafil (Levitra):
Vardenafil is a PDE5 inhibitor demonstrated to be effective and safe for treating ED in patients with Type 1 or Type 2 diabetes. Vardenafil is considered safe, but its risk profile includes absolute contraindication with nitrates. Common side effects reported include hot flush, rhinitis, nasal congestion, and headache.
- Other PDE5 Inhibitors (e.g., Avanafil, Mirodenafil, Udenafil):
Newer or less frequently studied PDE5 inhibitors have proven effective against placebo in clinical trials involving diabetic patients. These are generally effective, but their safety is monitored. Adverse events are similar to other PDE5 inhibitors, such as flushing, headache, and sinus congestion.
PDE5 inhibitors are crucial for managing ED in diabetic patients. Erectile Dysfunction medications like Sildenafil, Tadalafil, and Vardenafil are effective and generally safe. They can significantly improve the quality of life.
Where to Find Safe ED Pills for Men with Diabetes?
Safe ED pills for men with diabetes can be found through trusted providers like Fullhousepill, which offers a range of prescription and clinically tested products designed for treating ED with diabetes. Fullhousepill specializes in safe ED pills for men facing impotence in diabetes, helping improve sexual health while minimizing risks. Some of our best products include Cenforce 100 mg, Aurogra 100 mg, and Zeagra 100 mg, all formulated to provide effective ED treatment for diabetics. These medications work by enhancing blood flow and supporting erectile function, making them suitable options for men experiencing impotence or erectile dysfunction (ED) linked to diabetes. Always consult a healthcare professional before starting any prescription to guarantee safety and effectiveness in treating ED with diabetes.