Premature ejaculation (PE) is one of the most common forms of male sexual dysfunction, affecting nearly 20-30% of men globally. It is typically defined as ejaculation occurring within one minute of vaginal penetration, often with minimal stimulation and before voluntary control is achieved. PE may be lifelong (primary) or acquired (secondary), and it frequently leads to frustration, anxiety, and decreased sexual satisfaction for both partners.
The causes of PE are complex and multifactorial. Biological contributors include hypersensitivity of the penile nerves, abnormal neurotransmitter levels (especially serotonin), hormonal imbalances, and genetic predisposition. Psychological factors such as performance anxiety, depression, relationship stress, and early sexual experiences also play a critical role. In many cases, PE coexists with other sexual dysfunctions like erectile dysfunction, compounding its impact on quality of life.
Treatment approaches include behavioral strategies, psychological therapy, and pharmacologic interventions. Medications include on-demand SSRIs like dapoxetine, off-label SSRIs such as sertraline, topical anesthetics, and tramadol, all of which have shown effectiveness in delaying ejaculation. Long-term management may include cognitive behavioral therapy (CBT), pelvic floor muscle training, or medical interventions such as hyaluronic acid injections, botulinum toxin therapy, or selective dorsal neurectomy.
The following sections examine the causes, treatment options, and long-term management strategies for premature ejaculation.
What Is Premature Ejaculation?
Premature ejaculation (PE) is a common male sexual dysfunction that affects many men. It occurs when ejaculation happens earlier than desired. In most cases, this happens within about a minute of vaginal penetration and without the ability to delay or control it. The experience feels frustrating, disappointing, and may interfere with intimacy and sexual satisfaction. Over time, it leads to stress, low self-esteem, and strain in relationships.
PE is typically classified into two types. Lifelong premature ejaculation begins with a man’s first sexual experiences and happens consistently over time. In contrast, acquired premature ejaculation develops later, after a phase of normal sexual performance. While timing is an important factor, the main issue lies in the inability to control ejaculation. This makes it difficult for couples to enjoy a fulfilling and mutually satisfying sex life.
What Are the Causes of Early Ejaculation?
Early ejaculation is influenced by a mix of psychological and biological factors. Common psychological causes include performance anxiety, stress, depression, or a history of rushed sexual experiences. They trigger an overactive stress response that shortens the time to climax. On the biological side, factors such as hormonal imbalances, abnormal serotonin levels, or increased sensitivity in the penile nerves may contribute. In some cases, erectile dysfunction also leads to early ejaculation, as the fear of losing an erection may cause a man to rush intercourse.
What Are the Treatment Options Available for Premature Ejaculation?
Premature ejaculation is managed through a variety of treatment options, depending on its severity and underlying causes. Behavioral methods like the start-stop and squeeze techniques are often used to build better control over ejaculation during sexual activity. Medications such as selective serotonin reuptake inhibitors (SSRIs), commonly prescribed for depression, also increase the time to ejaculation as a side effect. Topical anesthetic creams or sprays work by numbing the penis slightly, reducing sensitivity and delaying climax. Another option is Tramadol, a pain reliever that has shown effectiveness in prolonging ejaculation when used off-label.
Nutritional supplements, such as zinc and magnesium, or herbal remedies may offer mild benefits. Lifestyle modifications, including stress reduction, regular exercise, and a proper diet, also support better sexual health. In cases where anxiety or relationship stress plays a role, psychological counseling is often effective. In cases where standard treatments are ineffective, more advanced options like selective dorsal neurectomy (SDN) or penile injections may be explored. These surgical interventions are typically considered only when other therapies have failed to provide relief.
In the sections below, we examine each of these treatment options in detail, including their mechanisms of action, effectiveness, and when they may be the right choice for managing premature ejaculation.
Behavioral Techniques
Behavioral techniques are structured, non-pharmacological strategies used to manage and overcome premature ejaculation (PE). These approaches aim to retrain the body’s natural response to sexual stimulation through repetition, self-control, and increased awareness of arousal levels. The goal is to delay ejaculation by learning how to recognize the sensation of an impending orgasm and respond to it in a controlled way. Unlike medications, behavioral methods involve no drugs or invasive procedures, making them a safe and accessible first-line treatment, particularly for men with mild to moderate PE.
These techniques are often most effective when psychological factors such as performance anxiety, low sexual confidence, or stress are contributing to the problem. They encourage a man to be more mentally and physically engaged during sexual activity, reduce pressure and build confidence over time. When practiced regularly, either alone or with a partner, they lead to significant improvements in ejaculatory control, sexual satisfaction, and relationship quality. Behavioral techniques are also used alongside other treatments, such as medications or counseling, for enhanced results.
The following are some of the most effective behavioral techniques used to manage premature ejaculation, each targeting different aspects of physical control and sensitivity.
Stop‑Start
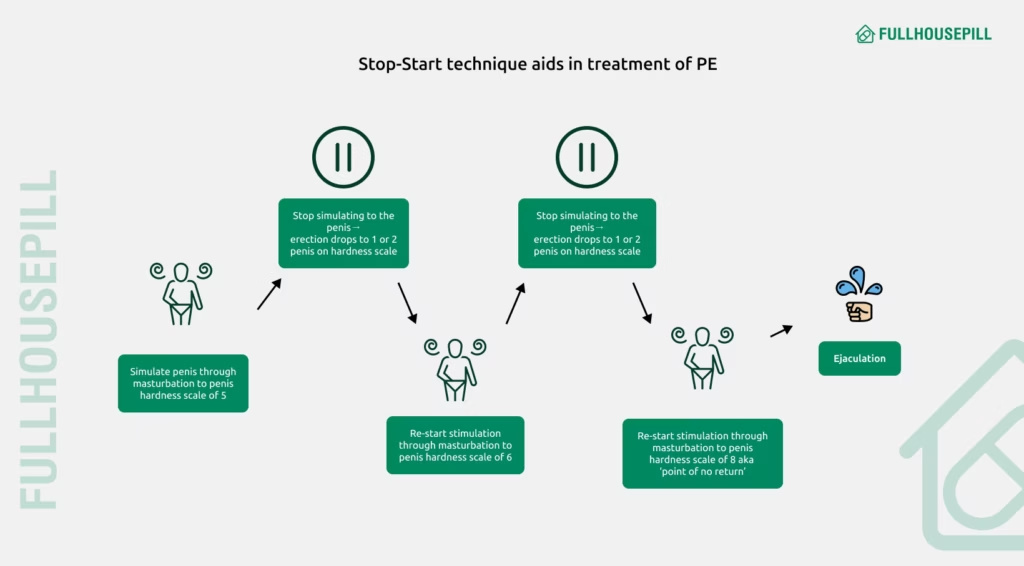
The stop-start technique is a behavioral therapy used to treat premature ejaculation (PE) by training individuals to gain better control over their ejaculatory reflex. It consists of repeatedly stimulating the penis until nearing climax, then pausing to let arousal decrease before continuing again. Over time, this method desensitizes the ejaculatory response and improves awareness of arousal levels.
This technique works by interrupting the build-up to orgasm, allowing the man to delay ejaculation consciously. Practiced regularly, either during partnered sex or masturbation, it gradually increases intravaginal ejaculatory latency time (IELT) and reduces anxiety related to sexual performance. It is often recommended as a first-line, non-pharmacological intervention for lifelong PE, particularly when combined with psychological counseling.
A study in PLOS One (2023) found that both the stop-start technique alone and combined with sphincter control training significantly increased IELT, improved sexual satisfaction scores, and reduced PE symptoms at 3 and 6 months. Additionally, the International Society for Sexual Medicine (ISSM) guidelines endorse behavioral strategies like the stop-start method as beneficial for men with PE, especially when medications are not preferred or suitable.
Squeeze Method
The squeeze method is a behavioral technique used to manage premature ejaculation (PE) by physically interrupting the ejaculatory reflex. It involves stimulating the penis until the man feels close to orgasm, then applying firm pressure, typically with the thumb on the underside and fingers on top, just below the glans (the tip of the penis) for a few seconds until the sensation of imminent ejaculation subsides. This process is repeated multiple times during a session to train greater ejaculatory control.
By temporarily decreasing arousal and interrupting the reflex to ejaculate, the squeeze method delays orgasm and increases awareness of arousal levels. Practiced consistently, it gradually extends intravaginal ejaculatory latency time and improves sexual confidence. It’s often recommended as a first-line, non-drug intervention, especially for men with lifelong PE or those preferring natural methods.
In a crossover trial published in the International Journal of Impotence Research (2001), the squeeze method increased median ejaculation time from 1 to 3 minutes in men with premature ejaculation. The technique involved pausing stimulation and applying pressure just below the glans when nearing climax. The study also noted that the squeeze method was well-tolerated, had no adverse effects, and was a practical, low-risk option for men preferring non-drug treatments for premature ejaculation.
Pelvic Floor Exercises (Kegels)
Pelvic floor exercises, commonly known as Kegel exercises, involve the repeated contraction and relaxation of the pelvic floor muscles, which play a crucial role in sexual function and ejaculatory control. These exercises are designed to strengthen the muscles that support the bladder, bowel, and the base of the penis.
Kegel exercises treat premature ejaculation by improving voluntary control over the muscles involved in ejaculation. Strengthening these muscles increases awareness and endurance, allowing men to delay orgasm during sexual activity better. Regular practice improves IELT, enhances sexual confidence, and reduces anxiety related to performance.
As per a study in Therapeutic Advances in Urology (2014), 12 weeks of pelvic floor muscle training led to significant improvements in men with lifelong premature ejaculation, increasing mean IELT from about 40 seconds to 146 seconds. Additionally, 82.5% of participants gained better ejaculatory control, with sustained benefits observed at a 6-month follow-up. The intervention was safe, well-tolerated, and offered a long-lasting, non-pharmacological solution.
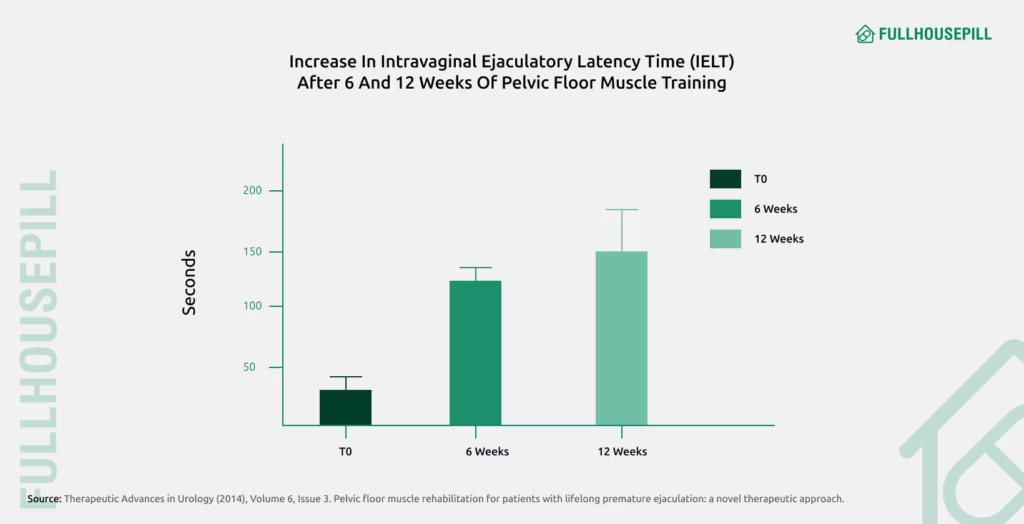
Another study in Physiotherapy (2019) also found that pelvic floor muscle exercises significantly improved ejaculatory control in men with premature ejaculation. Participants showed increased satisfaction and delayed ejaculation with no reported side effects.
Desensitizing Condom
Desensitizing condoms are specially designed male condoms that contain a low-dose topical anesthetic, such as benzocaine or lidocaine, applied to the inside surface. These agents work by gently numbing the penile skin, reducing sensitivity without completely dulling sensation. This mild numbing effect slows down sexual stimulation, giving men greater control over the timing of ejaculation. By lowering arousal buildup, these condoms delay climax and support longer-lasting intercourse. Unlike oral medications, they act directly at the site, taking effect almost immediately upon use and wearing off shortly after.
They are designed for on-demand use, making them a convenient and accessible option for men seeking to manage premature ejaculation without the need for daily pills or long-term behavioral training. Available without a prescription, desensitizing condoms offer a simple, non-invasive alternative that fits easily into a couple’s routine. They are especially useful for those who prefer a discreet, drug-free method with minimal risk of systemic side effects.
As per a clinical study in Translational Andrology and Urology (2022), using thickened condoms (three times the normal thickness) prolonged ejaculation time in men with premature ejaculation and reduced penile sensitivity by increasing vibration thresholds and slowing nerve conduction. The intervention also enhanced erection hardness and duration, as well as serum testosterone levels, although user comfort was somewhat diminished. Similarly, desensitized condoms coated with mild anesthetics like benzocaine work by dulling penile sensitivity, delaying climax and improving ejaculatory control. They offer a convenient, non-invasive option for men seeking on-demand relief from premature ejaculation.
Selective Serotonin Reuptake Inhibitors (SSRIs)
Selective Serotonin Reuptake Inhibitors (SSRIs) are a group of antidepressant drugs that work by enhancing the activity of serotonin, a key neurotransmitter in the brain. Serotonin is a neurotransmitter involved in mood regulation, but it also plays a key role in controlling ejaculation. SSRIs were originally developed to treat depression, but they are now widely used as a PE medication due to their ability to delay orgasm as a side effect.
In the treatment of premature ejaculation, SSRIs such as Dapoxetine, Paroxetine, Sertraline, and Fluoxetine are commonly prescribed. These medications work by increasing the amount of serotonin available in the nervous system, which slows down the ejaculatory reflex. Several clinical trials have shown that SSRIs increase intravaginal ejaculatory latency time (IELT), helping men gain better control during sex. Among these, Dapoxetine is the only SSRI specifically approved for on-demand use in premature ejaculation, making it a popular choice for men seeking fast-acting relief.
We now examine the specific SSRIs used to treat premature ejaculation, detailing their mechanisms, effectiveness, and when they are most appropriately prescribed.
Dapoxetine
Dapoxetine is a short-acting selective serotonin reuptake inhibitor (SSRI) specifically developed to treat premature ejaculation (PE) in men aged 18-64. Unlike traditional SSRIs used for depression, dapoxetine is taken on-demand, typically 1 to 3 hours before sexual activity, and is rapidly absorbed and eliminated, making it suitable for occasional use without long-term accumulation.
Dapoxetine works by increasing serotonin activity in the nervous system, which delays the ejaculatory reflex and improves control over ejaculation. It also enhances sexual satisfaction by reducing performance anxiety and increasing intravaginal ejaculation latency time (IELT).
An evidence-based review in Core Evidence (2012) concludes that dapoxetine effectively prolongs IELT when taken on-demand at doses of 30 mg or 60 mg. It also improves patient-reported outcomes like control over ejaculation, sexual satisfaction, and reduced distress. A meta-analysis in Clinical Therapeutics (2014) reviewed six randomized controlled trials and confirmed that dapoxetine effectively increased ejaculation time in men with premature ejaculation compared to a placebo. The 60 mg dose was more effective than the 30 mg dose. Side effects like nausea, dizziness, and headache were common but generally mild and well tolerated.
Paroxetine
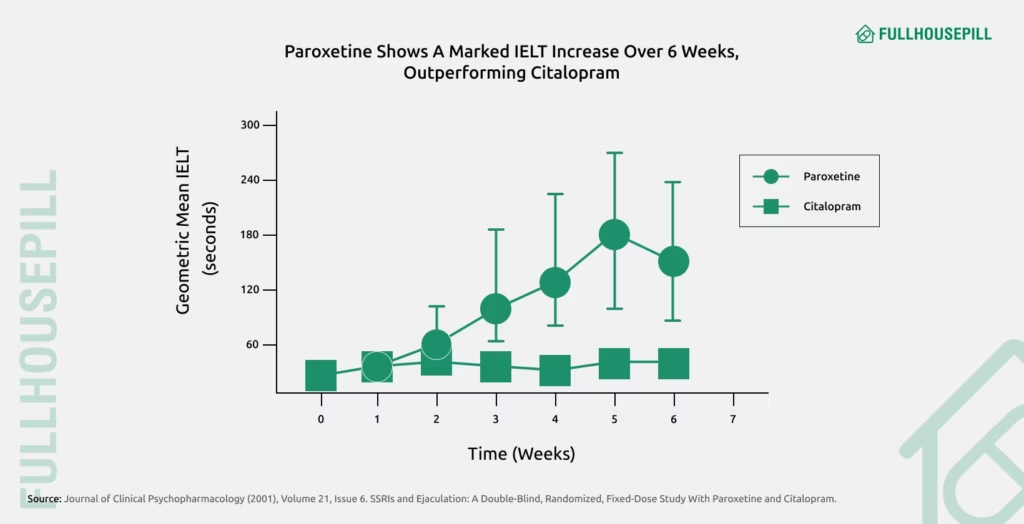
Paroxetine is a long-acting selective serotonin reuptake inhibitor (SSRI) commonly prescribed as an antidepressant. It has also been found effective in treating premature ejaculation (PE) by increasing serotonin levels in the brain, which delays the ejaculatory reflex. Unlike dapoxetine, paroxetine is typically taken daily and may take several days to build up therapeutic effects.
Paroxetine extends intravaginal ejaculatory latency time (IELT) and enhances ejaculatory control by modulating central serotonin pathways involved in orgasm and arousal. While not officially approved for PE, it is often prescribed off-label due to its proven efficacy.
An article in the Korean Journal of Urology (2014) discusses paroxetine as one of the most effective off-label pharmacological treatments for premature ejaculation. It highlights that daily use of paroxetine increases IELT, more so than other SSRIs. A randomized, double-blind study published in the Journal of Clinical Psychopharmacology (2001) compared the effects of paroxetine and citalopram on men with lifelong premature ejaculation. Paroxetine showed significantly greater improvement in delaying ejaculation compared to citalopram, showing a nine-fold increase in IELT, from about 18 seconds to 170 seconds.
Sertraline, Fluoxetine
Sertraline and fluoxetine belong to the class of SSRIs, widely prescribed for managing depression, anxiety, and related psychiatric conditions. However, both are frequently used off-label to treat premature ejaculation (PE) due to their ability to increase serotonin levels, which delays ejaculation by slowing down the ejaculatory reflex pathway.
These medications are typically taken daily rather than on-demand and may take 1-2 weeks to show noticeable effects on ejaculatory control. By prolonging the time to climax and improving control over ejaculation, sertraline and fluoxetine enhances sexual satisfaction and reduce distress in men with PE.
A double-blind, randomized study published in the Journal of Urology (1998) compared the effectiveness and safety of sertraline, fluoxetine, clomipramine, and placebo in men with premature ejaculation. Results showed that sertraline and clomipramine led to a greater increase in IELT compared to fluoxetine or placebo, indicating their superior efficacy. The study concluded that sertraline and fluoxetine are both effective SSRI options for PE, but sertraline may offer a stronger improvement in ejaculatory control.
Topical Anesthetics
Topical anesthetics are externally applied agents designed to temporarily reduce sensation by numbing the surface of the skin. In the treatment of premature ejaculation (PE), these products, usually in the form of creams or sprays, are applied to the penis before sexual activity to decrease sensitivity and delay ejaculation.
By partially numbing the nerve endings in the skin, topical anesthetics reduce the intensity of stimulation during sex, making it easier to control ejaculation. Commonly used agents include lidocaine, prilocaine, or a combination of both. Studies have shown that these anesthetics increase intravaginal ejaculatory latency time (IELT) when used correctly. To minimize the risk of reduced sensation for the partner, it’s recommended to apply the product 10-15 minutes before intercourse and wipe off any excess before penetration.
Next, we will examine the details of topical anesthetic products, focusing on their formulations, application methods, and role in the clinical management of premature ejaculation.
Lidocaine/Prilocaine Combinations
Lidocaine/prilocaine combinations are topical anesthetic creams commonly used in urology and dermatology to numb the skin and mucous membranes. These formulations, often referred to by brand names like EMLA (Eutectic Mixture of Local Anesthetics) cream, contain a balanced mixture of two local anesthetics, lidocaine and prilocaine, which work by blocking nerve signals in the applied area.
In the treatment of premature ejaculation (PE), these creams are applied to the glans penis approximately 20-30 minutes before intercourse, then wiped off before penetration. By partially numbing the penile skin, they reduce overstimulation and delay ejaculation. This localized effect enables men to prolong sexual activity without significantly diminishing overall sensation or pleasure.
According to a study in Andrologia (2002), a eutectic mixture of 4% lidocaine‐prilocaine applied to the penile glans for applying the lidocaine-prilocaine cream 20 minutes before intercourse was found to be the optimum timing for reducing sensitivity and effectively delaying ejaculation. This treatment led to a doubling of ejaculation latency compared to baseline, with minimal side effects reported. As per a systematic review and meta-analysis in Cureus (2023), topical anesthetic agents demonstrated efficacy in treating premature ejaculation. Across 11 randomized-controlled trials these agents consistently outperformed placebo and even oral medications like paroxetine and sildenafil in increasing ejaculatory control and satisfaction. Mild local side effects like burning and numbness were more frequent with topical use, but no serious adverse events were reported.
Delay Wipes
Delay wipes are disposable, pre-moistened wipes infused with a mild topical anesthetic, typically benzocaine or lidocaine, designed to reduce sensitivity in the glans penis. They are a discreet, fast-acting, and on-demand solution for men seeking to manage premature ejaculation (PE) without the use of oral medication or creams.
These wipes work by slightly numbing the penile surface, lower tactile sensitivity and delay the ejaculatory reflex during intercourse. Usually applied 5-10 minutes before sex and wiped off before penetration, delay wipes offer greater convenience and less mess than traditional topical creams. They allow men to prolong sexual activity while maintaining adequate sensation and intimacy.
A study published in the Journal of Men’s Health (2019) found that men using 4% benzocaine wipes experienced a statistically significant increase in ejaculation latency and sexual satisfaction after two months of use. No serious side effects were reported, and the wipes were well-tolerated, making them a practical and accessible treatment option for PE.
Tramadol
Tramadol is a medication that eases pain by acting on the central nervous system (CNS) to alter how the body senses discomfort. It is a synthetic opioid that acts on the CNS by activating μ-opioid receptors and blocking the reabsorption of serotonin and norepinephrine in the brain. These actions not only manage pain but also influence various neurological pathways involved in sexual function, including the ejaculatory reflex.
In recent years, tramadol has been explored as an off-label treatment for premature ejaculation (PE). Its ability to increase serotonin and norepinephrine levels is thought to delay ejaculation by modulating the central nervous system’s control over orgasm. Several studies have shown that taking a low dose of tramadol (typically 25-50 mg) one to three hours before sexual activity prolong intravaginal ejaculatory latency time (IELT). Unlike daily SSRIs, tramadol may offer faster results when used on demand.
A double-blind, placebo-controlled study published in The Journal of Urology (2006) showed that tramadol taken before sex increases ejaculation time in men with premature ejaculation, with higher doses doubling or nearly quadrupling the latency compared to placebo. Over half of the men treated with 50 mg and most with 100 mg achieved successful delay of ejaculation, though side effects like mild nausea and weak ejaculation were more common at higher doses. Despite some adverse effects, tramadol proved effective in managing premature ejaculation when used responsibly. A review of eight trials in BMC Urology (2015) found tramadol to be more effective than placebo and some other treatments in delaying ejaculation.
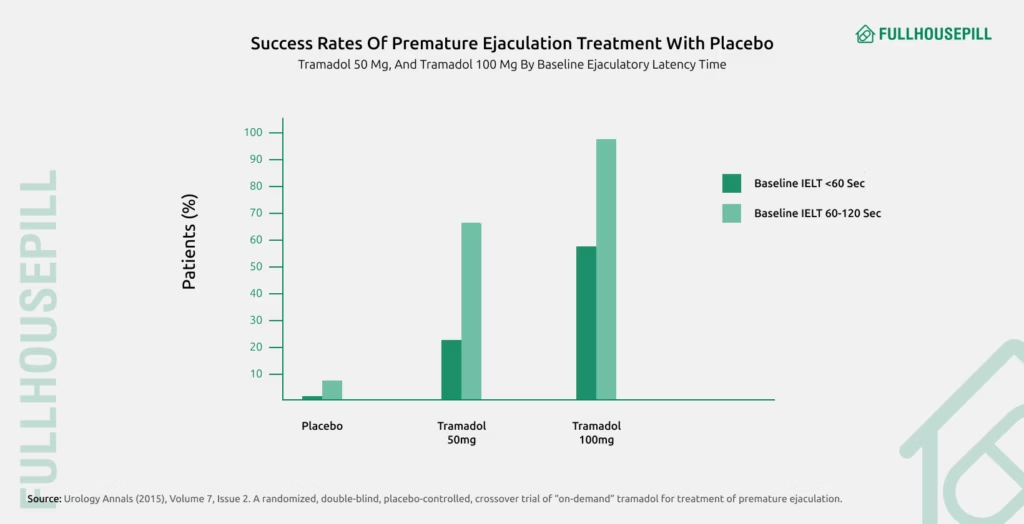
Tramadol delays ejaculation, but should be used only under medical supervision due to side effects and addiction risk.
Nutritional Supplements
Nutritional supplements are products that contain vitamins, minerals, amino acids, herbs, or other natural compounds intended to support bodily functions and overall well-being. They are commonly used to address nutritional deficiencies, improve energy levels, and support specific health concerns. Nutritional supplements are considered a complementary approach that may improve sexual performance and ejaculatory control through various physiological and psychological mechanisms. While they are not a primary or stand-alone treatment for PE, certain supplements are believed to support hormonal health, reduce stress, enhance nerve function, and increase stamina, all of which contribute to better control during sexual activity. Supplements are generally well-tolerated and accessible, making them an appealing option for men looking for natural ways to manage PE.
Common supplements used in PE management include zinc, magnesium, ginseng, and ashwagandha. Zinc and magnesium play a role in testosterone production and nerve function. Herbal supplements like ginseng and ashwagandha may reduce stress and improve sexual endurance.
We now examine key nutritional supplements that have been associated with improved ejaculatory control and their potential role in managing premature ejaculation.
Zinc
Zinc is an essential trace element involved in a wide range of bodily functions, including hormone regulation, enzyme synthesis, immune response, and cellular repair. It is important for male reproductive health, as it supports the production and regulation of testosterone, maintains prostate function, and aids in the proper functioning of the nervous system. These are essential factors for normal sexual performance and ejaculatory control. Zinc deficiency has been linked to reduced libido, lower testosterone levels, and impaired sperm quality, highlighting its fundamental role in male sexual well-being.
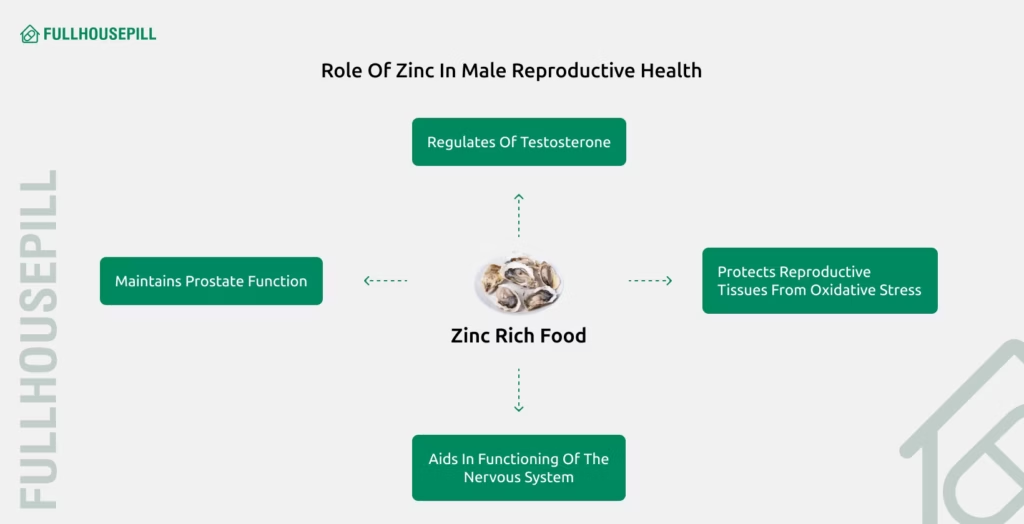
It also contributes to the maintenance of healthy nerve signaling pathways, which regulate the timing of ejaculation. It acts as a powerful antioxidant, protecting reproductive tissues from oxidative stress that impair muscle and nerve function in the pelvic region. By supporting both hormonal and neurological health, zinc improves ejaculatory control and overall sexual endurance, making it a promising natural option for men experiencing PE, particularly when used as part of a comprehensive nutritional plan.
A study published in Redox Report (2023) found that zinc supplementation improved sexual and erectile function by reducing oxidative stress and restoring key hormone levels, including testosterone, luteinizing hormone, and follicle-stimulating hormone. Zinc also enhanced nitric oxide signaling and antioxidant enzyme activity, contributing to better penile reflexes and performance. These findings highlight zinc’s potential role in supporting male sexual health by addressing oxidative and hormonal imbalances.
Magnesium
Magnesium is a key mineral involved in vital bodily functions like nerve signaling, muscle relaxation, hormonal balance, and cardiovascular regulation. It also supports healthy sexual function by influencing neurotransmitters and smooth muscle activity, both of which are crucial for ejaculatory control.
Men with premature ejaculation often have lower levels of magnesium in their seminal fluid, indicating a possible link between magnesium deficiency and poor ejaculatory regulation. Magnesium may delay ejaculation by promoting muscle relaxation, reducing nerve excitability, and improving overall sexual stamina.
A case-control study published in the British Journal of Urology International (2006) found that men with premature ejaculation had significantly lower levels of magnesium in their seminal plasma, despite normal blood magnesium. This suggests a local deficiency that could impair ejaculatory control through effects on nerve and muscle function. These findings support the idea that optimizing magnesium levels might benefit sexual function and delay ejaculation.
Herbal Remedies: Ginseng, Ashwagandha
Herbal remedies like Panax ginseng and Ashwagandha (Withania somnifera) are traditional adaptogenic herbs thought to enhance sexual health by improving stress resilience, hormonal function, and circulation.
A clinical trial published in Ayurvedic Journal of Health Sciences (2025) evaluated an eight-week course of standardized Ashwagandha root extract in men with sexual dysfunction. Participants reported noticeable improvements in sexual stamina, stress reduction, and ejaculatory delay, based on validated questionnaires. The study concluded that Ashwagandha is a well-tolerated, natural option to enhance sexual performance and potentially aid in managing premature ejaculation.
A comprehensive review in Food Supplements and Biomaterials for Health (2023) examined evidence on Panax Ginseng and concluded it has strong potential to enhance male reproductive health. It noted ginseng’s ability to improve sperm quality, boost libido, and support erectile function, effects which are driven by antioxidant actions, nitric oxide modulation, and hormonal regulation.
Together, these herbs offer promising natural support for sexual health and may serve as effective complementary options for managing premature ejaculation.
Lifestyle Modifications
Lifestyle modifications involve purposeful adjustments to daily routines and habits aimed at improving both physical and mental health. In the management of premature ejaculation (PE), adopting healthier lifestyle practices addresses underlying factors such as stress, fatigue, poor cardiovascular health, and low testosterone levels, all of which may contribute to reduced ejaculatory control.
Key lifestyle changes include engaging in regular physical activity, maintaining a balanced diet, getting adequate sleep, reducing alcohol intake, quitting smoking, and managing stress through techniques like meditation or deep breathing exercises. These habits improve blood circulation, enhance mood, stabilize hormone levels, and reduce anxiety, factors that play a significant role in sexual performance. While lifestyle changes may not serve as a standalone cure for PE, they are often recommended as part of a comprehensive treatment plan to support and enhance the effectiveness of medical or psychological therapies.
The following section outlines specific lifestyle changes that may support improved ejaculatory control and overall sexual health.
Regular Exercise
Regular exercise improves cardiovascular function, enhances endurance, and increases blood flow to the genital region, which enhances sexual stamina and control. It also supports hormonal balance, which naturally aids with premature ejaculation.
A systematic review of 12 randomized controlled trials in Cureus (2023) found that consistent aerobic exercise significantly improved male sexual function, as measured by the IIEF-5. It showed that exercise serves as a viable non-invasive strategy for enhancing sexual performance naturally.
Stress Management
Stress management through meditation, breathing exercises, and mindfulness techniques reduces anxiety, one of the major psychological contributors to premature ejaculation. Relaxation techniques help men stay mentally present and regulate arousal more effectively.
A randomized controlled trial published in the International Journal of Advanced Studies in Sexology (2022) involved men aged 18-60. The study found that a 60‑day mindfulness training program, featuring breathing exercises, meditation, and body scanning, reduced symptoms of premature ejaculation. It also improved sexual self-control compared to a no‑intervention group. The study concluded that mindfulness-based interventions are effective in alleviating PE, though further research is needed to isolate which specific techniques are most beneficial.
Dietary Improvements
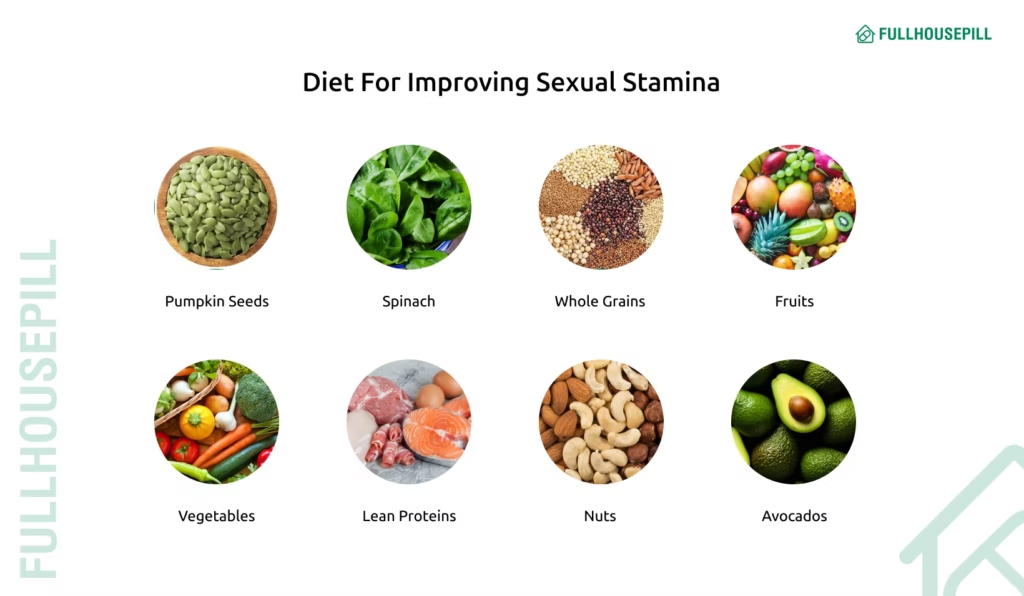
Improving your diet by focusing on foods rich in zinc and magnesium, like pumpkin seeds, spinach, whole grains, and legumes, enhance testosterone production, support nerve function, and promote muscle relaxation, all of which are important for sexual stamina and control. These nutrients play a key role in maintaining optimal sexual function and naturally delay ejaculation. Additionally, adopting a Mediterranean diet, which emphasizes fruits, vegetables, lean proteins, nuts, and healthy fats, has been associated with improved sexual health and ejaculatory control in several studies.
Avoiding Alcohol and Smoking
Avoiding alcohol and smoking is important, as both damage blood vessels, disrupt hormone balance, and impair nerve function, which worsens sexual dysfunction and premature ejaculation. Reducing or quitting these habits supports both short-term performance and long-term sexual health.
A cross-sectional study in the Indian Journal of Psychiatry (2007) found that premature ejaculation was among the most commonly reported sexual issues among men with alcohol dependence, appearing more frequently than low sexual desire and erectile dysfunction.
Psychological Counseling Vector
Psychological counseling involves structured, therapeutic conversations with a trained mental health professional to address emotional, behavioral, or cognitive issues. In the case of premature ejaculation (PE), counseling focuses on identifying and managing psychological factors such as performance anxiety, low self-esteem, relationship stress, or past negative sexual experiences that may contribute to the condition.
By helping individuals understand the emotional triggers behind PE, counseling improves sexual confidence, reduces anxiety, and fosters healthier communication with partners. Therapeutic approaches often involve cognitive-behavioral therapy (CBT), guided sex therapy sessions, and counseling aimed at improving partner communication through couples therapy. These methods aim to break the cycle of anxiety and poor control by reshaping thought patterns and improving emotional regulation. Counseling is particularly effective when PE is linked to stress, mental health concerns, or interpersonal issues, and it is often used alongside medical or behavioral treatments for a more comprehensive approach.
With this insight established, let us examine the specific counseling approaches commonly utilized to treat premature ejaculation.
Cognitive Behavioral Therapy
Cognitive Behavioral Therapy (CBT) is a structured, short-term psychological treatment that focuses on identifying and changing negative thought patterns, emotional responses, and behaviors. CBT in the treatment of premature ejaculation (PE) focuses on reducing performance-related anxiety, easing psychological stress, and enhancing control over sexual arousal and response.
CBT treats PE by targeting psychological factors such as low sexual confidence, fear of failure, and over-arousal. Through guided sessions, men learn coping strategies, relaxation techniques, and behavioral exercises (such as stop-start or squeeze methods) to gain better control over ejaculation and reduce distress.
A meta-analysis published in Andrology (2024) evaluated 1,243 men with PE and found that combining CBT with selective serotonin reuptake inhibitors (SSRIs) significantly improved outcomes compared to SSRIs alone. The combination led to longer intravaginal ejaculatory latency time (IELT), better ejaculatory control, and greater sexual satisfaction for both men and their partners. Importantly, the addition of CBT did not increase adverse effects, indicating it is a safe and effective adjunct treatment for PE.
Sex Therapy
Sex therapy is a specialized form of psychotherapy that addresses emotional, psychological, and relational issues related to sexual function and satisfaction. For men with premature ejaculation (PE), sex therapy explores underlying causes like anxiety, unrealistic expectations, or past trauma while teaching practical techniques to improve control and confidence during sex. Sex therapy treats PE by combining open communication, guided exercises, and mental reframing to reduce anxiety and improve intimacy.
For single individuals, sex therapy provides practical strategies such as stop-start techniques, guided masturbation, and cognitive reframing to improve control and reduce anxiety in solo or future partnered experiences. It also builds sexual confidence, making men feel more in control without relying on medication.
A study in the Journal of Sex & Marital Therapy (2007) explored the effectiveness of internet-based sex therapy for men with erectile dysfunction or premature ejaculation, using a 3-month email-guided program grounded in the Masters and Johnson model. Among those who completed the program, 67% reported improved sexual functioning, and nearly half maintained these improvements one month post-treatment. The results suggest online sex therapy is a promising and accessible treatment for premature ejaculation.
Couples Therapy
Couples therapy is a form of psychotherapy that focuses on improving communication, emotional intimacy, and relationship dynamics between partners. In the case of premature ejaculation (PE), couples therapy aids both partners to understand the condition, reduce blame or frustration, and work together to improve sexual satisfaction and emotional connection.
It treats PE by addressing relational stressors, performance anxiety, and mismatched expectations that may contribute to or worsen early ejaculation. Therapists may also guide couples through behavioral exercises and teach techniques to build trust and collaboration in the bedroom.
An article in Family Process (2022) highlights that couple-based interventions are effective in addressing sexual dysfunctions like PE. By involving both partners in therapy, particularly through behavioral and emotionally focused approaches, treatment outcomes may improve by fostering mutual understanding, support, and shared responsibility in the therapeutic process.

Surgical and Advanced Interventions
Surgical and advanced interventions refer to specialized medical procedures or technologies used when conventional treatments for premature ejaculation (PE) have not provided sufficient relief. These options are typically considered in severe or treatment-resistant cases and are aimed at altering nerve sensitivity or enhancing ejaculatory control through physical means.
One such approach is Selective Dorsal Neurectomy (SDN), which involves modifying the penile nerves responsible for sensation to reduce hypersensitivity. In some cases. Additionally, botulinum toxin (Botox) and hyaluronic acid injections into the penile muscles have been studied for their ability to reduce involuntary contractions and delay ejaculation. These interventions are generally reserved for men who do not respond to behavioral, pharmacological, or psychological treatments and should only be considered after thorough evaluation by a specialist.
A closer examination of these advanced interventions will clarify their mechanisms, potential benefits, and appropriate clinical use in the treatment of premature ejaculation.
Selective Dorsal Neurectomy (SDN)
Selective dorsal neurectomy (SDN) is a surgical technique aimed at reducing sexual hypersensitivity by selectively severing branches of the dorsal penile nerve. The procedure is designed to diminish penile sensation just enough to delay ejaculation while preserving erectile function.
SDN treats premature ejaculation by reducing sensitivity in the glans, thereby lengthening the ejaculatory reflex and enhancing control over climax. This nerve modulation enables a noticeably prolonged time before ejaculation, often without affecting erectile ability.
A systematic review and meta-analysis in the Journal of Sexual Medicine (2025) assessed the efficacy and safety of selective dorsal neurectomy or cryoablation (SDN/CA) for treating premature ejaculation across 7 clinical studies. The procedures significantly prolonged IELT by approximately 147 seconds and improved ejaculation control and sexual satisfaction, without negatively affecting erectile function. While the results are promising, there is a need for standardized surgical protocols and long-term follow-ups.
Botulinum Toxin Injections
Botulinum toxin-A (Botox) injections are an emerging treatment for premature ejaculation (PE), aiming to delay ejaculation by relaxing key pelvic muscles. By blocking acetylcholine release, Botox reduces contractions in muscles like the bulbospongiosus, and extends ejaculation time without impairing erectile function. At times, treatment may target the ischiocavernosus or frenulum muscles.
Two recent meta-analyses on Botulinum toxin-A for PE offer contrasting conclusions. A review in the International Journal of Impotence Research (2025) of three RCTs found no significant long-term benefit in IELT or Premature Ejaculation Profile (PEP) scores at 1, 3, or 6 months. Another study in a Chinese journal – Zhonghua Nan Ke Xue (2018) reported modest short-term improvements at 1 month that diminished over time. Both studies noted mild, transient side effects but confirmed no negative impact on erectile function. The key difference lies in interpretation; one rejects Botox for routine use due to limited durability, while the other sees it as a short-term option for select patients. Overall, Botox shows limited and temporary benefit, warranting further large-scale, standardized research.
Hyaluronic Acid Injections
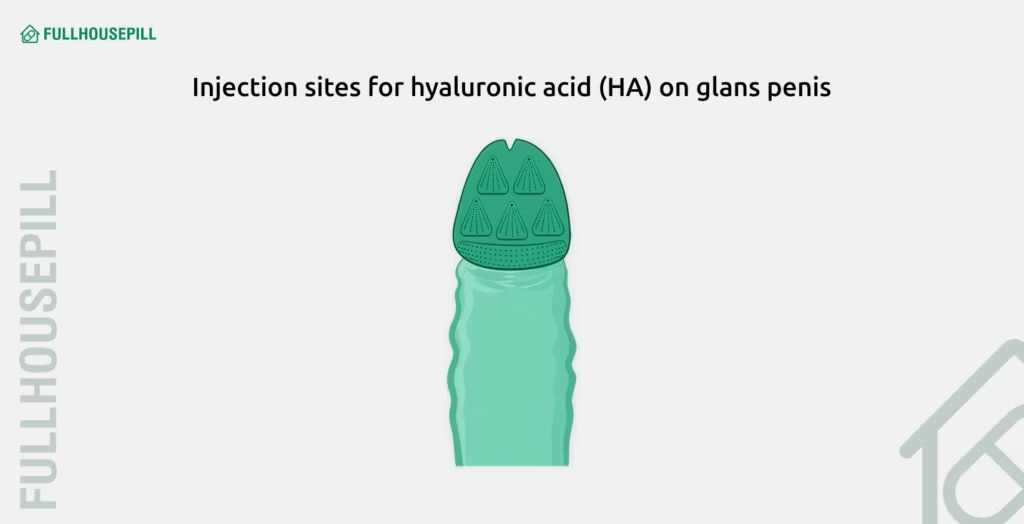
Hyaluronic acid (HA) injections involve injecting a biocompatible filler into or around the glans penis to create a cushioning layer that reduces sensitivity. It works by adding volume to the glans penis, creating a physical buffer that reduces sensitivity to friction during intercourse. This decreased tactile stimulation delays the ejaculatory reflex. The result is improved control over ejaculation without affecting erection quality.
A randomized, single-blind, crossover study in the International Journal of Impotence Research (2019) evaluated the effectiveness of HA injections into the glans penis for treating premature ejaculation in 30 men. The results showed that HA significantly increased IELT compared to saline, and also improved PE-related symptom scores. These effects persisted for up to 9 months in many participants. The procedure was generally safe, causing only mild side effects that resolved on their own without medical intervention. Overall, HA injections were found to be a safe and moderately effective intervention for improving ejaculatory control.
Managing premature ejaculation effectively requires a personalized approach and medical advice, especially when it involves surgical interventions.
How to cure premature ejaculation naturally?
Natural remedies for premature ejaculation focus on physical control, psychological conditioning, and hormone balance. Premature ejaculation (PE) can often be managed through non-pharmaceutical methods that enhance stamina and arousal control. Pelvic floor exercises (Kegels) improve the strength of muscles involved in ejaculation. Regular aerobic activity boosts blood flow and sexual endurance. Practicing the start-stop technique or the squeeze technique during intercourse or solo sessions can retrain ejaculatory reflexes. Mindfulness or breathing exercises reduce performance anxiety, which is a common trigger for PE. Managing stress and improving sleep also help regulate serotonin, a neurotransmitter involved in ejaculatory timing.
What are the foods to cure PE?
PE-supportive foods promote serotonin levels, improve blood flow, and balance hormones.
- Oats – Increase serotonin naturally and may support ejaculatory control.
- Bananas – Contain bromelain and B vitamins that support testosterone levels.
- Pumpkin seeds – Rich in zinc, crucial for testosterone production.
- Avocados – Provide vitamin B6 and folic acid, which help with energy and endurance.
- Spinach – Boosts magnesium and nitric oxide, which aid in arousal and endurance.
- Dark chocolate – Contains flavonoids and phenylethylamine, enhancing mood and arousal.
- Watermelon – Natural source of citrulline, which promotes smooth muscle relaxation.
These PE-friendly foods support both physical and mental stamina during sexual activity.
How to last longer in bed?
Training, dietary changes, and mental focus help you last longer during sex. To last longer during sex, practice techniques that delay ejaculation like the start-stop or squeeze method. Strengthen the pelvic floor with regular Kegel exercises. Use desensitizing condoms or apply a numbing cream (with a doctor’s guidance). Eat foods that support stamina, such as whole grains, leafy greens, and protein-rich meals, and avoid stimulants like nicotine and excessive caffeine. Reducing anxiety through meditation or therapy also improves control. Improving foreplay and communication with your partner can extend the experience and reduce pressure.
Does sildenafil help in premature ejaculation?
Sildenafil may indirectly help by reducing anxiety and improving confidence, but it is not a primary treatment for PE. Sildenafil, the active ingredient in Viagra, is primarily used to treat erectile dysfunction, not premature ejaculation. However, some men report delayed ejaculation as a secondary effect of the drug. By improving erection firmness and reducing performance anxiety, sildenafil may help extend the duration of intercourse. That said, clinical evidence is mixed, and doctors usually prescribe selective serotonin reuptake inhibitors (SSRIs) like dapoxetine for PE instead.
Can premature ejaculation cause pregnancy?
Yes, pregnancy is possible even if ejaculation happens early or outside full penetration. Premature ejaculation does not prevent pregnancy. If ejaculation occurs near or inside the vagina, even during brief or partial penetration, sperm can travel into the uterus. Pre-ejaculate (pre-cum) may also contain viable sperm, especially if ejaculation occurred recently beforehand. Couples trying to avoid pregnancy should use contraception, regardless of ejaculation timing.
