Sperm fertility depends on how well sperm survive and fertilise an egg. Thickness and strength play a big role in this process because they reflect semen motility and vitality. Healthy sperm are linked to better chances of conception, while poor quality lowers fertility. Several natural factors can impact sperm health. Lifestyle and diet, along with sleep and stress, all play a role. Heavy smoking leads to reduced sperm counts, while alcohol consumption causes higher rates of morphologically abnormal sperm. This was supported by the Journal of International Medical Research.
Exercise and proper nutrition improve sperm parameters. According to Frontiers in Endocrinology, Outdoor aerobics significantly improved sperm volume in infertile patients. Balance is important because sperm quality can decline with age and unhealthy habits; however, changes in diet and lifestyle may help restore function. Intense exercise can lead to changes in semen quality; the effects vary depending on the type, intensity, and duration of the physical activity. This article highlights how sperm fertility works, what thickness and strength mean, and natural and medical ways to improve sperm quality. It also includes the role of food, lifestyle and supplements that help to enhance sperm health.
What is Sperm Fertility?
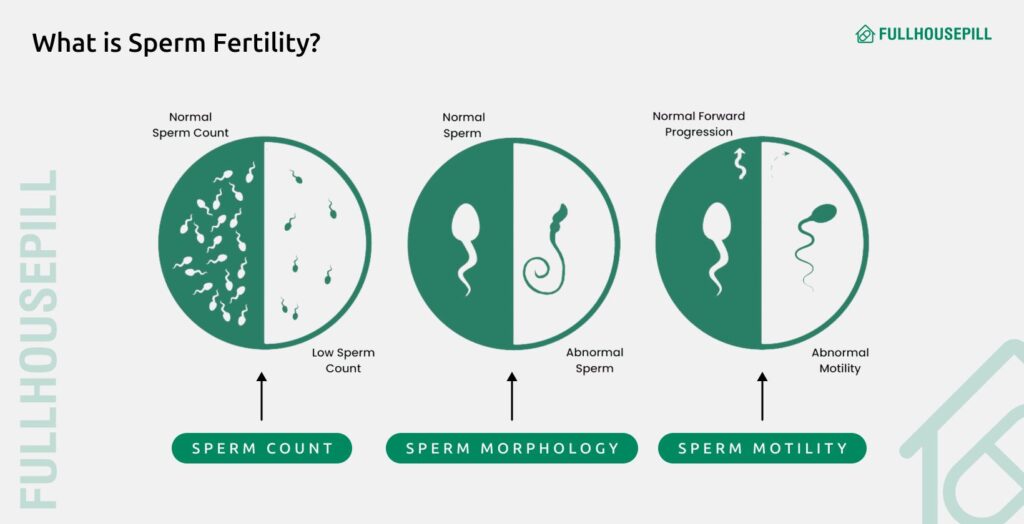
Sperm fertility means the ability of sperm to fertilise an egg and start a pregnancy. It depends on measurable qualities such as thickness, strength, count, motility, and morphology. These factors together decide whether sperm can travel through and survive in the female reproductive system and reach the egg. They determine whether sperm successfully reach the egg.
Thickness- The Thickness of seminal fluid, also called semen viscosity, is the ability to liquefy after ejaculation. Normal semen should become less viscous and ≤2 cm when semen is dropped through the pipette thread measurement after liquefaction, as per WHO (2021), Laboratory Manual for the Examination and Processing of Human Semen.
Strength- Strength describes the energy and activity of sperm. Strong sperm swim forward with force and last longer. Weak sperm often stop before reaching the egg, lowering fertility potential.
Count- Count is the total number of sperm in one millilitre of semen. A normal sperm concentration is at least 15 million sperm per millilitre or greater, according to the World Health Organisation (WHO) 2021. Anything lower is called low sperm count and can reduce the chances of fertilisation.
Motility- Motility refers to movement. Healthy ejaculation should contain at least 42% of sperm cells that show some form of movement (total motility) and a minimum of 30% that show progressive motility according to WHO (2021), Laboratory Manual for the Examination and Processing of Human Semen (6th ed, Sections 5.2–5.4). Reduced motility is one of the most common reasons for male infertility.
Morphology- Morphology is the shape and structure of sperm. A healthy sperm has a smooth oval head, a midpiece that provides energy, and a tail that drives movement. 4% of sperm should be normally shaped according to the WHO (2021) Laboratory Manual for the Examination and Processing of Human Semen.
What Does Sperm Thickness & Strength Mean?
Sperm thickness refers to semen viscosity, while strength relates to how well sperm function and survive. Both matter for fertility because they affect how easily sperm travel through the female reproductive tract. Semen viscosity is the resistance of semen to flow after liquefaction. Normally, semen becomes liquid within 30 minutes of collection and no later than 60 minutes after ejaculation, as reported by WHO (2021). The World Health Organisation (WHO) define normal viscosity as a thread shorter than 2 cm when semen is dropped from a pipette. This increased viscosity can hinder sperm motility and is considered an abnormal finding in semen analysis.
Thick semen is usually not a cause for concern. It can be influenced by hydration, hormone levels, and how often ejaculation happens. However, very thick or clumpy semen may point to problems. Hyperviscous semen often reduces sperm motility and may lower total sperm count. Some men with low sperm count still have semen that appears normal, so thickness alone does not confirm fertility status.
Thick semen can sometimes happen because of dehydration, infrequent ejaculation, or lifestyle habits like heavy alcohol use and long periods of sitting. Hormonal imbalance may also play a role. Thick, clumpy semen can point to inflammation or infection in the prostate or seminal vesicles. These issues can increase oxidative stress, which damages sperm DNA and may reduce fertility, as per the World Journal of Men’s Health.
Lifestyle also plays a role. Excessive smoking and alcohol consumption are associated with reduced sperm count and increased sperm abnormalities. According to European Urology, in a study of 62 healthy men, semen samples were analysed by light and transmission electron microscopy to assess the effects of smoking and alcohol on sperm quality. Heavy smoking (>20 cigarettes/day) was linked to reduced sperm count, while moderate to high alcohol intake (≥15.4 g/day) was associated with more morphologically abnormal sperm. Electron microscopy showed no ultrastructural changes from smoking, but alcohol intake increased abnormalities in sperm nuclei and plasma membranes. These findings suggest that smoking lowers sperm quantity, whereas alcohol primarily affects sperm morphology.
Sedentary lifestyle and physical inactivity are risk factors associated with infertility. In a multicenter case-control study published in PLoS ONE, of 302 adults, infertility in men was linked to physical inactivity and excess fat mass. In women, it was associated with sedentary behaviour, high fat mass, and low fat-free mass. Physical activity level was not related to fertility in women, and sedentary time was not linked in men. These findings suggest that inactivity and sedentary behaviour may be independent risk factors for infertility, highlighting the importance of lifestyle and body composition in prevention and treatment.
Semen that is thin or watery at ejaculation can be a sign of low sperm count, as per WHO (2021), Laboratory Manual for the Examination and Processing of Human Semen, 6th ed., section on oligospermia. This condition, called oligospermia, reduces the chances of fertilisation.
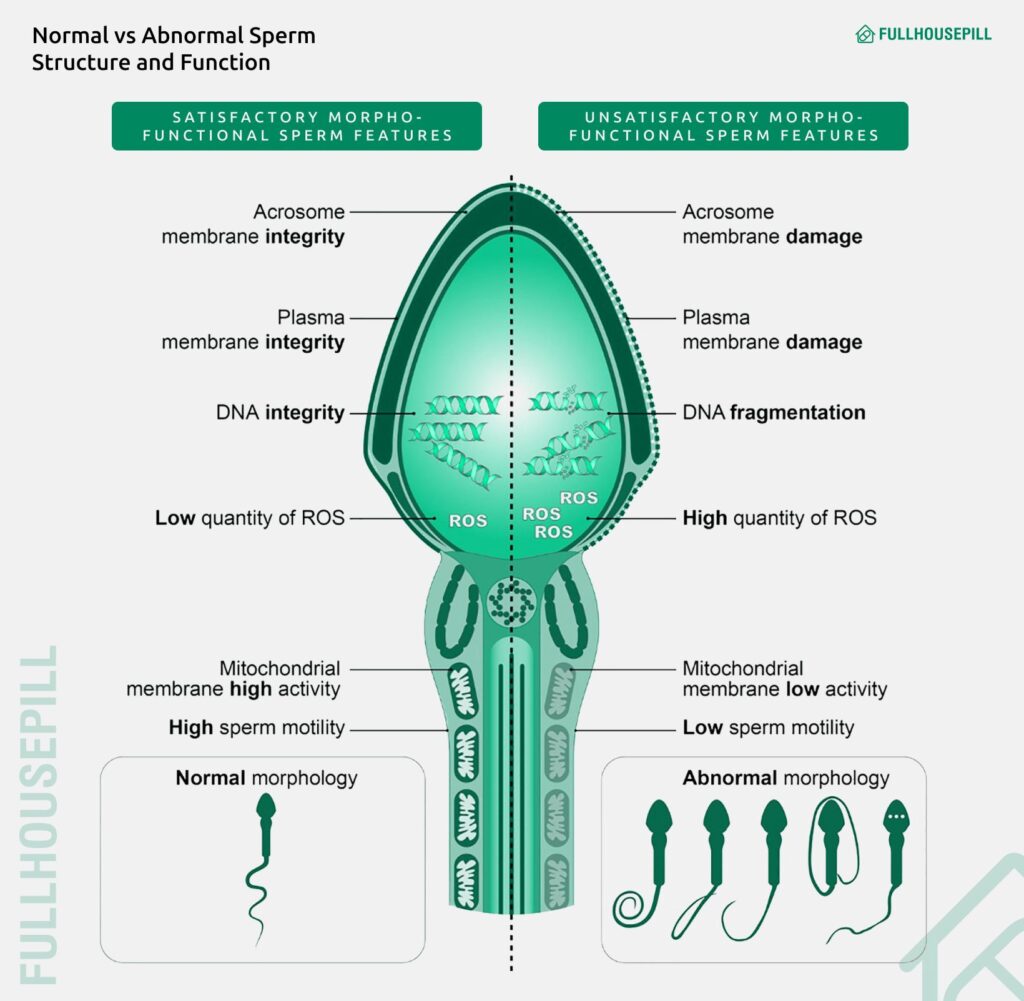
Sperm strength describes three features: motility, vitality, and DNA integrity. Strong sperm move forward with energy, survive longer, and carry stable genetic material. Weak sperm may fail to reach or fertilise the egg. These qualities together are considered essential markers of male fertility.
What Factors Naturally Affect Sperm Thickness and Strength
Sperm thickness and strength are shaped by several natural influences. These include hormones, age, hydration, and genetic differences. Being around pesticides, lead, and other toxins can affect sperm quantity and quality. Regular exercise and avoiding tobacco products can help improve sperm quality. Each factor plays a clear role in how semen flows and how sperm perform.
Hormonal Influences (Testosterone, FSH, LH)
Hormones control how semen forms and how sperm mature. For instance, testosterone fuels sperm development. FSH and LH help regulate this process in the testes. Decreased and increased levels of hormones could adversely affect semen profile and sperm DNA integrity, which leads to severe male infertility. High LH typically reflects testicular dysfunction rather than directly impairing motility or morphology. This was supported by Oduwole, O. O., et al (2021), International Journal of Molecular Sciences.
Age-Related Changes and Decline Patterns
Sperm health is also shaped by age. Men may still produce sperm throughout life, but the quality declines with time. Sperm motility and morphology show a steady decline after the age of 40, according to Human Reproduction. Volume and motility gradually decline after the age of 40 years.
Hydration Status and Semen Consistency
Hydration directly affects semen thickness. If the body is not properly hydrated, there may be less fluid in the semen, causing it to be thick or clumpy. Proper hydration helps semen stay fluid, supporting better sperm movement through the female reproductive tract.
Individual Genetic Variations and Baseline Fertility
Genetics set the baseline for semen quality. Some men naturally produce semen with a thicker or thinner consistency. These inherited traits shape how sperm look and act, even when all else is normal, according to the Journal of Human Reproductive Sciences. Genetic disorders affect male fertility by their adverse influence on testicular volume, hormone levels, and sperm concentration. It has been reported that men with a genetic variation in CHDH (rs12676) had reduced sperm motility or asthenospermia according to PLOS ONE.
How to make sperm thicker and stronger
Sperm quality can be improved through a mix of lifestyle changes, nutrition, supplements, and, in some cases, medical care. The body responds well to healthy habits and balanced nutrition, which often enhance semen thickness and sperm vitality. Research shows that physical activity, stress control, and good diet patterns contribute to stronger sperm and better fertility outcomes.
Lifestyle Changes to Improve Sperm Quality
Lifestyle changes can directly improve sperm quality if maintained over time, with evidence showing benefits from regular exercise, quality sleep, healthy weight, and avoiding toxins and heat exposure. Modifiable habits like diet, activity, risk substance use, stress control, and weight have a measurable effect on sperm count, motility, and DNA integrity as per the Asian Journal of Andrology.
Exercise and Testosterone
Moderate exercise boosts sperm health by improving hormone balance, reducing oxidative stress, and supporting better semen quality. Outdoor aerobic exercise helped increase sperm volume in men with infertility. Other types of exercise improved sperm motility and total sperm count. Resistance training improved sperm shape (morphology), and cycling exercise increased sperm concentration. This was supported by Song, W., et al (2025), Frontiers in Endocrinology. Intense or excessive endurance sports, however, are linked with DNA fragmentation and lower sperm quality. Exercise leads to fluctuations in the secretion of gonadotropins and androgens. According to the International Brazilian Journal of Urology, research shows that hCG increases energy, libido and strength in men with low testosterone.
Sleep and Stress Management
Sleep is crucial for normal reproductive function. Sleep deprivation might be related to impaired semen quality, according to Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. Stress influences semen quality through neuroendocrine factors influencing spermatogenesis. Stress leads to increased levels of glucocorticoids, leading to decreased rates of testosterone. According to Fertility and Sterility, men who experienced two or more stressful life events in the past year, compared with those who experienced no stressful events, had a lower percentage of motile sperm. In a study of 193 men from the Child Health and Development Studies, researchers examined the impact of stress on semen quality. Higher perceived stress scores were linked to lower sperm concentration, motility, and morphology. Men reporting two or more stressful life events in the past year had significantly reduced motility and fewer morphologically normal sperm compared to those with no stressful events, though sperm concentration was unaffected. Job strain showed no association. Overall, perceived stress and life stressors, but not work-related stress, were associated with impaired semen quality.
Maintain a Healthy Weight
Obesity is directly correlated with lower sperm count and poorer motility, as confirmed in recent systematic reviews by Bocu, K., et al. (2024), Asian Journal of Andrology. Weight loss through dietary changes and increased physical activity improves hormone balance and semen quality.
Avoid Smoking, Alcohol, and Excessive Heat
Smoking reduces sperm motility and total sperm count. Alcohol intake worsens sperm motility and morphology, as reported by Heliyon. Any heat source, such as saunas, hot tubs, sitting with a laptop on the lap, or tight underwear, can lower sperm count and quality. Thus, it is suggested to avoid or minimise these exposures.
Foods for Thicker and Stronger Sperm
Diet plays one of the most important roles in male fertility. The nutrients a man consumes directly influence sperm thickness, motility, and ability to fertilise an egg. Sperm cells are highly sensitive to vitamins, minerals, healthy fats, and antioxidants found in food. These elements protect sperm DNA, regulate hormones, and build strong cell membranes. Foods high in zinc, omega-3 fatty acids, antioxidants, and vitamin D have shown the most consistent benefits for sperm health. Men looking to improve sperm quality should focus on nutrient-dense foods that support healthy sperm production and motility. Research confirms that certain food groups provide measurable benefits for sperm count, movement, and shape.
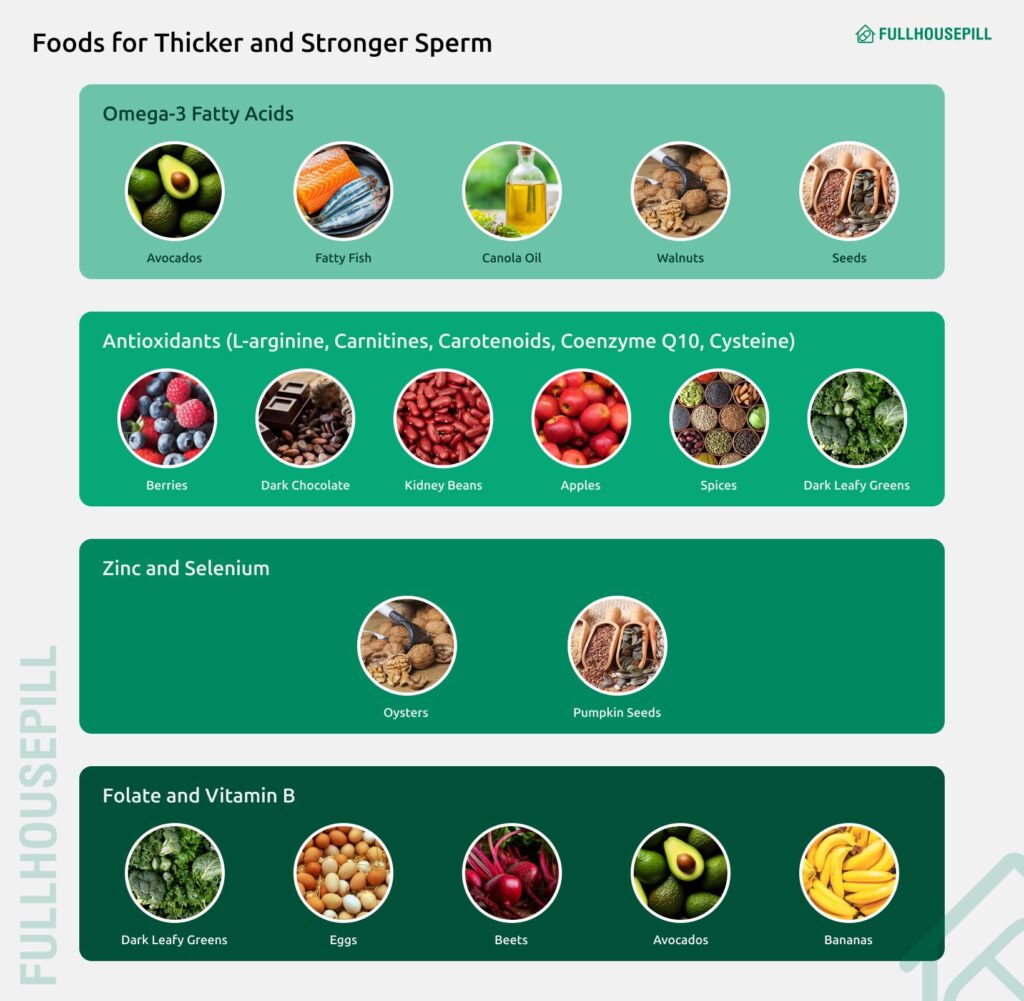
Zinc-Rich Foods (Oysters, Beef, Beans)
Oysters, beef, and beans contain high levels of zinc, which directly support sperm production and testosterone levels. Zinc supplementation significantly increases sperm volume, motility, and percentage of normal morphology. According to the Journal of Trace Elements in Medicine and Biology, men with higher seminal plasma zinc concentrations have better sperm quality
Omega-3 Sources (Fish, Walnuts, Chia Seeds)
Fatty fish like salmon and sardines provide omega-3 fatty acids that enhance sperm concentration and total count. Eating 75 grams of walnuts daily improves sperm vitality, motility, and morphology, as documented by Robbins et al (2012) in Biology of Reproduction. It showed significant improvements in sperm parameters with reduced chromosomal abnormalities. Although these improvements do not necessarily translate into complete restoration of fertility.
Antioxidant Foods (Berries, Garlic, Dark Chocolate)
Berries, garlic, and dark chocolate supply antioxidants that protect sperm DNA from oxidative damage and improve motility. Clinical trials demonstrate that antioxidant supplementation reduces sperm DNA fragmentation by approximately 19% according to the Journal of Assisted Reproduction and Genetics. Men with high DNA fragmentation levels show the greatest improvements from antioxidant-rich foods.
Vitamin D Foods (Eggs, Fortified Milk, Salmon)
Eggs, fortified milk, and salmon provide vitamin D, which supports hormone balance and sperm function. Vitamin D supplementation significantly improves total sperm motility, progressive motility, and normal morphology in infertile men. This is confirmed as per the Arab Journal of Urology: An International Journal. Men with vitamin D deficiency show measurably lower sperm quality.
Mediterranean Diet Benefits
Following a Mediterranean eating pattern rich in vegetables, fish, nuts, and olive oil correlates with better semen parameters. This includes sperm count, concentration, and motility, according to the Asian Journal of Andrology. Studies consistently show that higher adherence to Mediterranean diet patterns improves multiple measures of sperm quality.
Supplements That Help Sperm Health
Supplements can make a real difference in male fertility when used alongside a healthy diet and lifestyle. They provide concentrated doses of nutrients that are sometimes difficult to get in enough amounts from food alone. These compounds work by improving testosterone balance, protecting sperm DNA, and strengthening semen quality. Over time, they help make sperm thicker, stronger, and more motile.
D-Aspartic Acid
D-aspartic acid naturally occurs in the testes and plays a role in testosterone and hormone production. Supplementation with 2.6 grams daily for 90 days significantly increased sperm concentration. It also improved motility, according to Advances in Sexual Medicine. The amino acid works by stimulating luteinizing hormone and testosterone release through the hypothalamic-pituitary-gonadal axis.
Vitamin C
Vitamin C protects sperm from oxidative DNA damage and improves motility in some studies. Research shows that Oral supplementation of vitamin C in infertile men might improve sperm motility and sperm morphology, as per the Journal of Medicinal Food. However, results are mixed, with some trials showing no improvement, suggesting individual variation in response.
Selenium
Selenium supports sperm motility and protects against oxidative damage through selenoprotein function. Clinical trials show selenium supplementation improves sperm concentration and morphology in infertile men, as Ahmadi, S., et al (2016), International Journal of Reproductive Biomedicine. The combination of selenium with vitamin E improved sperm parameters in 52.6% of cases, induced spontaneous pregnancy in 10.8%, and showed a mean 4.3% semen improvement. This was supported by Moslemi, M. K., & Tavanbakhsh, S. (2011), International Journal of General Medicine.
Zinc and Folic Acid Combination
Daily supplementation with zinc sulfate and folic acid over several months may boost sperm count in men with fertility issues. According to Fertil Steril, Combined zinc sulfate (66 mg) and folic acid (5 mg) daily for 26 weeks increases total normal sperm count by 74% in subfertile men (total motile count).
Ashwagandha, Shilajit, and Other Herbs
Ashwagandha root extract (675 mg daily) for 90 days produces remarkable improvements. It led to an increase in sperm count, semen volume, and motility in oligospermic men. This was demonstrated in a randomised controlled trial published in Evidence-Based Complementary Medicine by Ambiye et al (2013). The herb also increased testosterone by 17% and luteinizing hormone by 34%.
According to Andrologia, Shilajit (100 mg twice daily) for 90 days improved sperm count by 61.4%. It also increased motility by 12.4-17.4% and normal sperm count by 18.9% in oligospermic patients. Shilajit also increased testosterone by 23.5% and decreased oxidative stress markers in semen.
Drinks That May Support Sperm Health
Beverages contribute more to male fertility than many realise. The type and quality of fluids consumed can influence semen consistency, sperm vitality, and the body’s overall reproductive balance. Proper hydration supports normal semen viscosity, while antioxidant-rich drinks help protect sperm cells from oxidative damage. Nutrient-dense options such as green tea, pomegranate juice, and milk or fortified plant-based alternatives provide compounds that aid hormone regulation and sperm function. Including these drinks as part of a balanced lifestyle can naturally enhance sperm thickness and strength.
Hydration and Semen Consistency
Proper hydration is essential for semen production and quality. When the body becomes dehydrated, semen becomes thicker and more viscous. This can reduce sperm motility.
Green Tea (Antioxidants)
Green tea extract at appropriate concentrations provides protective antioxidant benefits for sperm health. Human studies demonstrate that green tea extract at 1.0 ng/mL protects sperm motility and reduces DNA fragmentation when used as a cryoprotectant, as per the Asian Journal of Andrology. However, the effects observed in laboratory preservation settings should not be directly extrapolated to dietary consumption. Higher concentrations of certain antioxidants may reduce sperm motility.
Pomegranate Juice
Pomegranate juice slightly improves sperm quality through its high antioxidant content. Drinking pomegranate juice increases reduced glutathione (GSH) levels and decreases lipid and protein oxidation in human blood, as per the Food and Chemical Toxicology. Clinical studies suggest the use of pomegranate extracts in the therapy of erectile dysfunction, as reported by Evidence-Based Complementary and Alternative Medicine.
Milk and Fortified Plant-Based Alternatives
According to Fertil Steril, Low-fat dairy products, particularly skim milk, show positive associations with sperm health. These benefits appear linked to dairy protein content rather than fat. However, full-fat dairy and cheese may negatively affect sperm parameters.
Plant-based diets correlate with sperm health, with vegan men demonstrating significantly higher percentages of rapid progressive and motile sperm according to the Journal of Human Reproductive Sciences. Plant-based milk alternatives may support reproductive health by providing antioxidants and avoiding potentially harmful compounds found in conventional dairy.
Medical Treatment Options
Medical treatment becomes essential when lifestyle changes, diet, and supplements are not enough to improve sperm health. Modern reproductive medicine offers structured solutions that can identify and address underlying issues. The most common approaches include semen analysis for low sperm count diagnosis, hormonal therapies such as hCG, and advanced assisted reproductive technologies like IVF and ICSI. These interventions provide men with proven options to boost fertility and improve their chances of fatherhood.
- Low Sperm Count Diagnosis (Semen Analysis)
Semen analysis is the baseline diagnostic tool. It measures key sperm parameters to determine the severity and type of sperm abnormality. The results help doctors tailor treatment plans and monitor progress.
- hCG and Hormonal Treatments
For men with hormonal imbalances like hypogonadotropic hypogonadism, treatments such as human chorionic gonadotropin (hCG) and gonadotropins stimulate natural sperm production. According to Current Urology, hCG therapy can increase Semen Parameters and Pregnancy Rate after Varicocelectomy.
- Assisted Reproductive Technologies (ART): IVF and ICSI
When natural conception is not possible due to severe sperm issues, assisted reproductive technologies such as in vitro fertilisation (IVF) and intracytoplasmic sperm injection (ICSI) offer effective alternatives. ICSI is particularly successful for male-factor infertility by directly injecting a single sperm into the egg. High fertilisation and pregnancy rates are reported with these procedures, as per Human Reproduction.
How Long Does It Take to Improve Sperm Quality?
It usually takes about three months to improve sperm quality. This timeframe matches the sperm production cycle, which lasts around 64 to 74 days, followed by a short maturation period.
Sperm quality improves when lifestyle changes are maintained consistently. Eating an antioxidant-rich diet with foods like leafy greens and berries, exercising regularly, quitting smoking, limiting alcohol, and keeping a healthy weight all support sperm production. Heat exposure from hot tubs, saunas, or laptops on the lap should be minimized, as high temperatures impair sperm health. Environmental toxins, such as pesticides and heavy metals, can also negatively affect sperm quality.
You can improve sperm quality by adopting healthy habits. Eat a balanced diet, exercise moderately, and manage your weight. Quit smoking to lower DNA damage in sperm. Reduce alcohol intake to support hormone balance. Avoid frequent heat exposure to the testicles.
You should consult a doctor if fertility concerns persist. Medical evaluation can rule out underlying conditions and provide targeted treatment if necessary.
How to Make Sperm Stronger for Pregnancy?
Sperm can be made stronger by improving lifestyle, diet, and, in some cases, with supplements or medical help. Regular exercise, good sleep, and a nutrient-rich diet improve motility and semen thickness. According to Advances in Nutrition, increased intake of selenium and zinc, omega-3 (ω-3) fatty acids, and CoenzymeQ10 (CoQ10) have been positively related to sperm quality.
Can Watery Sperm Get a Woman Pregnant?
Yes, watery sperm can still cause pregnancy if it contains enough healthy and motile sperm. Semen consistency alone does not decide fertility, since even thinner semen may carry sperm capable of reaching the egg. While watery sperm may indicate lower sperm count or motility, it does not necessarily prevent conception. Even with a lower sperm count, a few healthy sperm can still reach and fertilise an egg.
Can Pre-Seminal Fluid Lead to Pregnancy?
Yes, pre-seminal fluid can sometimes lead to pregnancy, but the chances are lower compared to semen. Pre-ejaculate itself usually contains little or no sperm, so on its own, it rarely causes conception, as per Human Fertility.
Can erectile dysfunction cause low sperm quality?
Erectile dysfunction (ED) does not directly cause low sperm quality. ED affects the ability to achieve or maintain an erection for intercourse, while sperm quality depends on production and maturation within the testes.
ED and poor sperm quality can be connected through shared underlying causes. Hormonal imbalances such as low testosterone, advancing age, and certain medications can affect both erectile function and sperm health. Systemic illnesses and anatomical issues may also contribute to both conditions. In some cases, ED acts as a symptom of a deeper health problem that simultaneously reduces sperm production or quality.
Ejaculatory problems linked to ED can reduce the frequency of sexual activity, which in turn lowers the chances of conception. However, the sperm itself is not damaged by ED alone.
Can generic Viagra improve male fertility?
Yes, generic Viagra (sildenafil) can help indirectly by treating erectile dysfunction (ED) and allowing regular intercourse. Viagra reduces stress linked to infertility. Stress can harm sexual function. By improving erections, Viagra creates a better chance for natural conception. The effect of Viagra on sperm quality is unclear. Some studies show that PDE5 inhibitors like Viagra may improve sperm motility and shape. Other studies show no major change in sperm count, movement, or structure. Viagra is not a fertility drug. It does not directly improve sperm quality. Its main role is to help men with ED have intercourse.
Can generic Cialis improve male fertility?
Yes, generic Cialis tablet may improve male fertility by supporting better sperm quality. Research shows it can increase motility, improve sperm shape, and raise semen volume. It also appears to have positive effects on spermatogenesis without harming reproductive hormones.
Tadalafil helps sperm health in several ways. Daily use can increase the total and fast motility of sperm. It can raise the percentage of nemasperms, which are sperm with a normal shape. It can also boost semen volume, which may support fertility potential.
The benefits are most visible with low-dose daily treatment. Studies show that Tadalafil is safe and does not negatively affect reproductive hormones. Some men may see a clear improvement in sperm parameters, while others may not. More research is needed before Tadalafil can be considered a reliable fertility therapy.
Tadalafil is not a fertility drug. It is approved for erectile dysfunction and benign prostatic hyperplasia. Its role in infertility treatment is off-label. Men should consult a doctor before using it for fertility support and discuss other established options like clomiphene or assisted reproductive techniques.
What is the best ED medicine for sperm motility?
The best ED medicine for sperm motility is not clearly defined, but research shows mixed results with sildenafil citrate (Viagra). Laboratory studies found that sildenafil citrate can increase the number and velocity of progressively motile sperm. These effects were seen in both high-quality (90%) and lower-quality (45%) sperm fractions. Sildenafil also increased the percentage of acrosome-reacted sperm, which is a key step in fertilization.
However, the same studies caution that sildenafil may have adverse effects on male fertility. The increase in premature acrosome reactions could reduce the fertilizing potential of sperm, even if motility appears improved. Cialis (tadalafil) has also been studied. Evidence suggests that daily low-dose tadalafil may improve sperm motility, semen volume, and sperm shape without major adverse hormonal effects.
