Over the counter (OTC) ED pills? Viagra Alternative
Over-the-counter (OTC) ED pills are increasingly popular among men looking for alternatives to prescription medications like Viagra. While prescription drugs […]
Black Friday Sale is Live . Flat 25% OFF !!

Sexual dysfunction in men disrupts the ability to experience satisfying sexual activity due to persistent problems in desire, arousal, ejaculation, or orgasm. These issues are medically recognized and often linked to physical illness, psychological distress, hormonal imbalance, or lifestyle-related vascular damage. Erectile dysfunction (ED) is the most prevalent, affecting up to 37% of men aged 70–75, followed by premature ejaculation, low libido, and delayed ejaculation. Each condition impairs one or more phases of the male sexual response cycle and often causes emotional or relational distress. According to the Global Study of Sexual Attitudes and Behaviors, approximately 28% of men aged 40–80 years report at least one form of sexual dysfunction, underscoring its global and age-related impact.
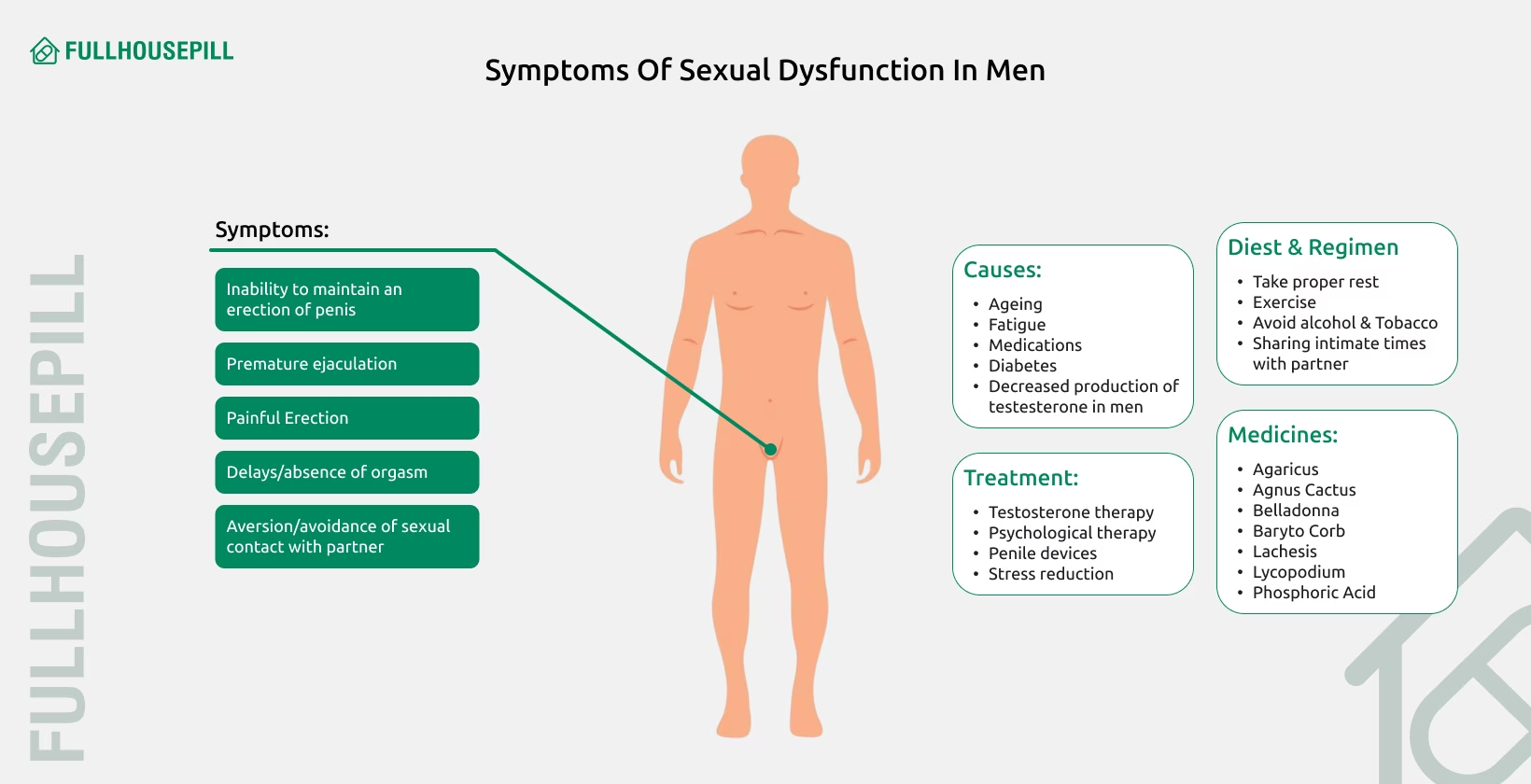
Clinically, sexual dysfunction is distinguished by its persistence, frequency, and the distress it causes. Diagnosis follows structured criteria from authoritative sources like DSM-5 and ICD-11, which classify disorders based on duration, severity, and etiology. Treatments range from PDE5 inhibitors and testosterone therapy to psychotherapy, pelvic-floor training, and novel interventions like topical gels or shockwave therapy. Natural remedies, such as Panax ginseng, Kegel exercises, and stress-reduction techniques, are also used for mild or early-stage dysfunction. By combining evidence-based treatments with personalized care, sexual function can often be restored or significantly improved.
Sexual dysfunction in men refers to a persistent or recurrent difficulty in one or more phases of the sexual response cycle that prevents satisfactory sexual performance. The male sexual response cycle consists of four stages: desire, arousal, orgasm, and resolution. DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition) and ICD-11(International Classification of Diseases, Eleventh Revision) both classify sexual dysfunctions, but they apply different diagnostic frameworks and terminologies.
Male sexual function follows a physiological cycle with four distinct phases:
Dysfunction in any stage may result in conditions such as erectile dysfunction, delayed ejaculation, or diminished sexual desire. Sexual dysfunction differs from infertility, although both may affect reproductive health. A man may retain normal sexual function despite being infertile. Low testosterone is not synonymous with sexual dysfunction, although hormonal imbalance may contribute to it.
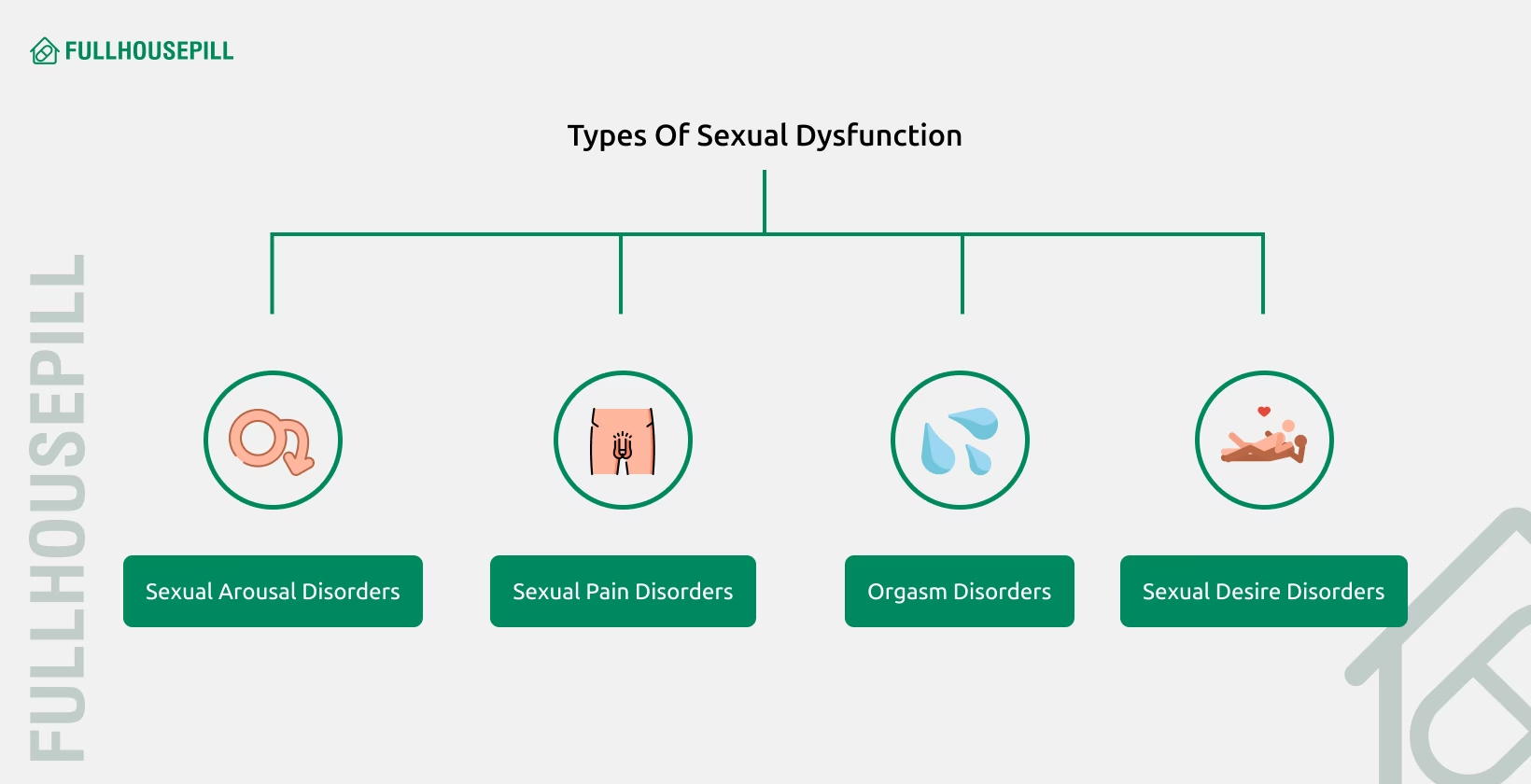
Sexual dysfunctions in men are medically classified according to the stage of the sexual response cycle they disrupt: desire, arousal, orgasm, or resolution. These conditions may be lifelong or acquired and can arise from physiological, psychological, relational, or pharmacological causes. Below are the five major types of male sexual dysfunction, each defined by clinical features and diagnostic consensus. The following table introduces the five key types of male sexual dysfunction, with definitions followed by detailed descriptions of their causes, prevalence, and treatments.
| Type | Definition |
|---|---|
| Erectile Dysfunction (ED) | Persistent or recurrent inability to attain or maintain an erection sufficient for intercourse. |
| Premature Ejaculation (PE) | Ejaculation that occurs shortly after penetration and with minimal stimulation. |
| Low Sexual Desire | Ongoing deficiency or absence of sexual thoughts, interest, or responsiveness. |
| Delayed Ejaculation (DE) | Prolonged or failed ejaculation despite sufficient arousal and sexual activity. |
| Peyronie’s Disease (PD) | Acquired penile condition involving fibrotic plaques that cause curvature, pain, or dysfunction. |
Erectile dysfunction is the consistent or recurrent inability to achieve or maintain an erection with sufficient rigidity for penetrative sexual activity. It is the most prevalent male sexual dysfunction, affecting both physical and emotional wellbeing. ED arises from a breakdown in the vascular, neurological, hormonal, or psychological systems that control penile tumescence. Most cases are attributed to organic causes like atherosclerosis, diabetes mellitus, or medication use. Psychogenic ED occurs less frequently and typically affects younger men or those experiencing acute mental distress.
ED does not include disorders such as priapism or penile deformities. The condition is strongly associated with modifiable risk factors including smoking, obesity, metabolic syndrome, and sedentary lifestyle. Vascular health plays a central role in erectile function, making ED a sentinel marker for cardiovascular disease.
Treatment starts with identifying and addressing the underlying cause. First-line therapy includes oral PDE5 inhibitors like sildenafil, which enhance nitric oxide–mediated vasodilation in penile blood vessels. In cases unresponsive to medication, mechanical aids (e.g., vacuum erection devices), intraurethral alprostadil, penile injections, or implants may be used. According to epidemiological studies, ED affects approximately 18% of men aged 50 to 59 years, increasing to 37% among those aged 70 to 75 years.
Premature ejaculation is a common male sexual disorder characterized by rapid ejaculation, typically within one minute of vaginal penetration, accompanied by a lack of control and personal or relational distress. The condition affects men across age groups and may be either lifelong (primary) or acquired after a period of normal ejaculatory control. Although time-based definitions vary, the International Society for Sexual Medicine defines PE as ejaculation that occurs too quickly and with minimal stimulation, usually before or shortly after penetration.
Men with PE often express frustration, embarrassment, and avoidance of sexual intimacy. PE is sometimes confused with anxiety-related arousal or high sexual excitability, but the clinical distinction lies in the lack of voluntary control and consistent rapid climax. The typical intravaginal ejaculation latency time in the general male population is about 4 to 8 minutes, whereas PE often occurs within 60 seconds.
Management of PE includes behavioral techniques such as the start-stop method, use of topical anesthetic creams, and pharmacological interventions like dapoxetine, a short-acting selective serotonin reuptake inhibitor. Cognitive behavioral therapy is also effective in reducing psychological distress associated with the condition.
Low sexual desire, or hypoactive sexual desire disorder, is a persistent or recurrent reduction in sexual interest, thoughts, fantasies, or receptivity, which leads to distress or impaired relationships. This condition may be global or situational and can occur with or without physical arousal dysfunction. In men, it often reflects hormonal imbalances, particularly low serum testosterone, though psychological and relational factors are frequently involved. Fatigue, aging, chronic illness, and certain medications, especially SSRIs and antipsychotics, also reduce libido.
Men with reduced libido may experience frustration or confusion about their diminished sexual motivation, which can have a cascading effect on relationship satisfaction and self-esteem. Low desire may follow stressful life events or emotional disconnection from a partner.
Effective treatment depends on identifying reversible causes. Testosterone replacement therapy is indicated for men with confirmed hypogonadism. Otherwise, management includes adjusting or stopping libido-suppressing medications, addressing mental health conditions like depression, and employing psychotherapy or couples therapy when appropriate. Despite its prevalence, low desire in men remains underdiagnosed due to cultural taboos and lack of standardized diagnostic criteria.
Delayed ejaculation is a persistent or recurrent delay in, or absence of, orgasm and ejaculation despite normal sexual arousal and activity, causing distress to the individual. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), DE is diagnosed when a man experiences marked delay, infrequency, or absence of ejaculation in at least 75% of partnered sexual encounters for a minimum of six months. The Third International Consultation on Sexual Medicine sets the intravaginal ejaculation latency time threshold at more than 20–25 minutes for DE diagnosis.
DE can be lifelong (primary) or acquired, and situational or generalized. Lifelong DE may be idiopathic, whereas acquired DE is often associated with pharmacological causes such as selective serotonin reuptake inhibitors, neurologic conditions, or psychological blocks. Though less prevalent than other ejaculatory disorders, DE significantly affects sexual confidence and partner intimacy.
Management includes identifying and stopping causative medications, psychosexual counseling, or desensitization training. In rare cases, vibrating stimulation devices or pharmacological support may be considered. While occasional delays are common, only 1% of men report lifelong DE, and about 4% report acquired persistent DE.
Peyronie’s disease is an acquired fibrotic disorder of the penis, characterized by the development of collagen-rich plaques in the tunica albuginea, resulting in abnormal curvature, penile pain, and often erectile dysfunction. This condition typically presents in two phases. The acute inflammatory phase involves pain and evolving curvature, while the chronic phase features stable deformity without pain but possible erectile rigidity issues. The disease often impairs penetrative function, leading to anxiety and avoidance of sexual activity.
The etiology is believed to involve repeated penile trauma during erection, leading to dysregulated wound healing and overexpression of transforming growth factor-beta 1 (TGF-β1). PD shares pathophysiological features with Dupuytren’s contracture and other fibrotic conditions. Some known risk factors for this condition include diabetes, aging, smoking cigarettes, and a history of penile injury. Diagnosis is primarily clinical but may be confirmed with penile ultrasound. Treatment varies depending on the phase. In early stages, oral therapies like pentoxifylline or vitamin E may be trialed. Intralesional injections with collagenase are effective in some cases. Severe or functionally limiting curvature may require surgical correction such as plication, grafting, or penile prosthesis placement. Epidemiological studies estimate the prevalence of PD between 3% and 9%, rising with age and comorbid ED.
Symptoms depend on the type of dysfunction, but all lead to problems with sexual satisfaction or sexual performance. Most men experience one or more of the following signs: reduced sexual desire, difficulty getting or keeping an erection, early ejaculation, or delayed or absent orgasm. Some conditions also cause physical changes in the penis, such as pain or curvature, especially during an erection. Common symptoms of male sexual dysfunction include the following:
Each dysfunction arises from a range of physical, psychological, and behavioral causes. The table below summarizes the major causes for each type:
| Type | Key Symptoms |
|---|---|
| Erectile Dysfunction (ED) | Trouble getting or keeping an erection, reduced firmness, incomplete erections |
| Premature Ejaculation (PE) | Ejaculation within one minute, lack of control, distress during intercourse |
| Low Sexual Desire | Lack of interest in sex, few or no sexual thoughts, emotional detachment |
| Delayed Ejaculation (DE) | Long time to ejaculate, inability to climax, frustration during sex |
| Peyronie’s Disease (PD) | Curved or painful erection, hard lumps in the penis, difficulty with penetration |
Replace “Sexual Dysfunction psychogenic factors” with “Causes of sexual dysfunction”
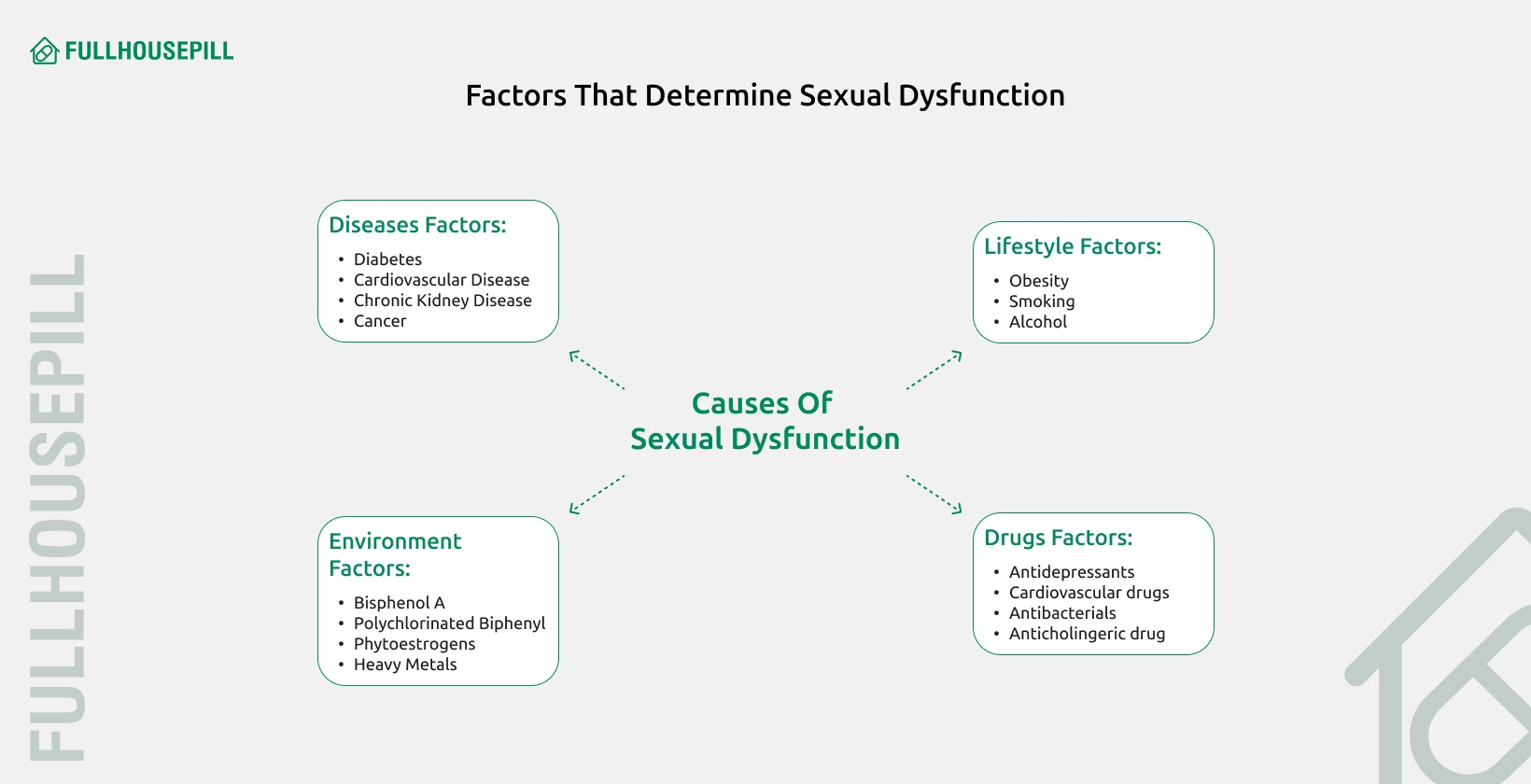
Sexual dysfunction in men may arise from physical illness, psychological distress, unhealthy lifestyle choices, or medication side effects. Many cases involve a combination of these causes. Physical conditions such as diabetes, hypertension, and cardiovascular disease can damage blood vessels and nerves, leading to arousal or erection problems. Psychological disorders like depression, anxiety, and post-traumatic stress disorder (PTSD) may suppress libido or interfere with arousal.
Unhealthy habits such as smoking, excessive alcohol consumption, and physical inactivity increase the risk of sexual dysfunction. Some medications, especially selective serotonin reuptake inhibitors (SSRIs) and antihypertensives, are also known to affect sexual function by altering hormonal or neurological pathways.
Excessive pornography consumption may contribute to sexual problems in otherwise healthy men. This phenomenon is referred to as porn-induced erectile dysfunction (PIED). It involves difficulty achieving or maintaining an erection during real-life sex due to desensitization to normal sexual cues, often caused by frequent viewing of high-stimulation pornographic material. Men with PIED typically report strong erections while watching porn but struggle during partner-based sexual activity. This condition can overlap with low desire or arousal-based dysfunction.
| Dysfunction Type | Physical Causes | Psychological Causes | Other Contributing Factors |
|---|---|---|---|
| Erectile Dysfunction (ED) | Cardiovascular disease, diabetes, hypertension, obesity, low testosterone, nerve damage | Depression, anxiety, performance pressure | Smoking, alcohol, medications (e.g., SSRIs, antihypertensives), excessive porn consumption |
| Premature Ejaculation (PE) | Penile hypersensitivity, prostatitis, serotonin imbalance | Anxiety, early sexual conditioning, relationship stress | Lack of experience, low self-esteem |
| Low Sexual Desire | Low testosterone, chronic illness, medication side effects | Depression, stress, relationship conflict | Fatigue, aging, boredom |
| Delayed Ejaculation (DE) | Nerve damage, diabetes, pelvic surgery, use of SSRIs or antipsychotics | Performance anxiety, fear of pregnancy, trauma | Alcohol use, low arousal from partner |
| Peyronie’s Disease (PD) | Penile trauma, abnormal wound healing, collagen overproduction | Anxiety, embarrassment from deformity | Age, Dupuytren’s contracture, diabetes, smoking |
Age impacts male sexual function by reducing testosterone, weakening blood flow, and decreasing erectile tissue responsiveness. These changes develop gradually over time and may appear earlier or more severely in men with chronic conditions such as diabetes or cardiovascular disease. The difference between natural aging and disease-related decline is crucial in identifying whether the dysfunction requires medical treatment.
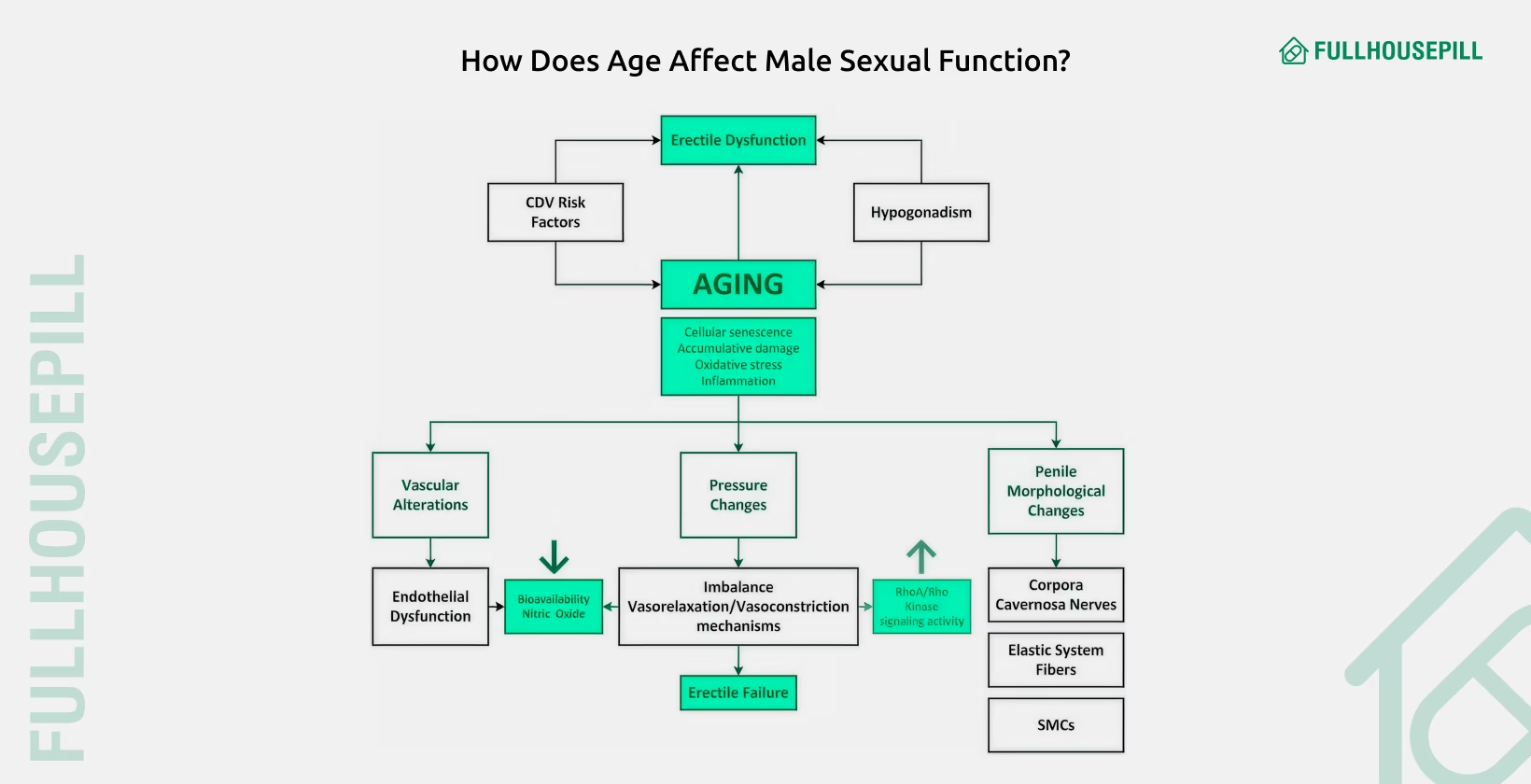
Normal aging involves slow declines in sexual function. Testosterone levels, particularly free testosterone, begin to drop in the late 30s or early 40s. This leads to lower libido, decreased morning erections, and reduced sexual energy. The arteries that supply the penis become stiffer with age, and the erectile tissues lose elasticity. Erections may become slower to develop, less firm, or harder to maintain. These shifts are common in older men and often do not interfere significantly with sexual satisfaction.
In contrast, pathological decline occurs when medical conditions accelerate damage to the vascular and nervous systems involved in sexual response. Men with diabetes, hypertension, or high cholesterol often experience more severe and earlier erectile issues. These effects go beyond what is expected from age alone. Many of these dysfunctions can be reversed or improved with proper medical care.
Aging also affects the ability of the penile tissues to respond to nitric oxide, the chemical that allows smooth muscle relaxation and blood engorgement. As a result, older men may need more direct stimulation and may face longer delays between sexual arousal and erection. Nerve conduction also slows with age, which adds to this latency.
Libido tends to decline as testosterone falls, with men losing about 1% of total testosterone per year after age 40. By their 40s, many men have already experienced a 10% decline from peak levels. These hormonal shifts may lower sexual interest and motivation for intimacy. However, not all men lose their libido with age. Many maintain healthy sexual desire due to stable mental health and strong relationships. When testosterone drops below clinical thresholds, a condition known as hypogonadism, sexual desire often declines sharply.
Chronic conditions make sexual dysfunction more likely and more difficult to treat. Men with diabetes are nearly three times more likely to experience erectile problems. High blood sugar damages the nerves that trigger an erection and narrows the arteries that supply the penis. Other conditions, like atherosclerosis and high blood pressure, further reduce blood flow. Medications used to treat these diseases, including SSRIs, beta-blockers, and diuretics, can also affect arousal, ejaculation, or desire.
The relationship between age and erectile dysfunction is well-established. Many older men experience ED due to a combination of natural aging and chronic illness. In some cases, lifestyle changes and medication adjustments can restore function. In others, treatment for underlying conditions is needed before sexual performance improves.
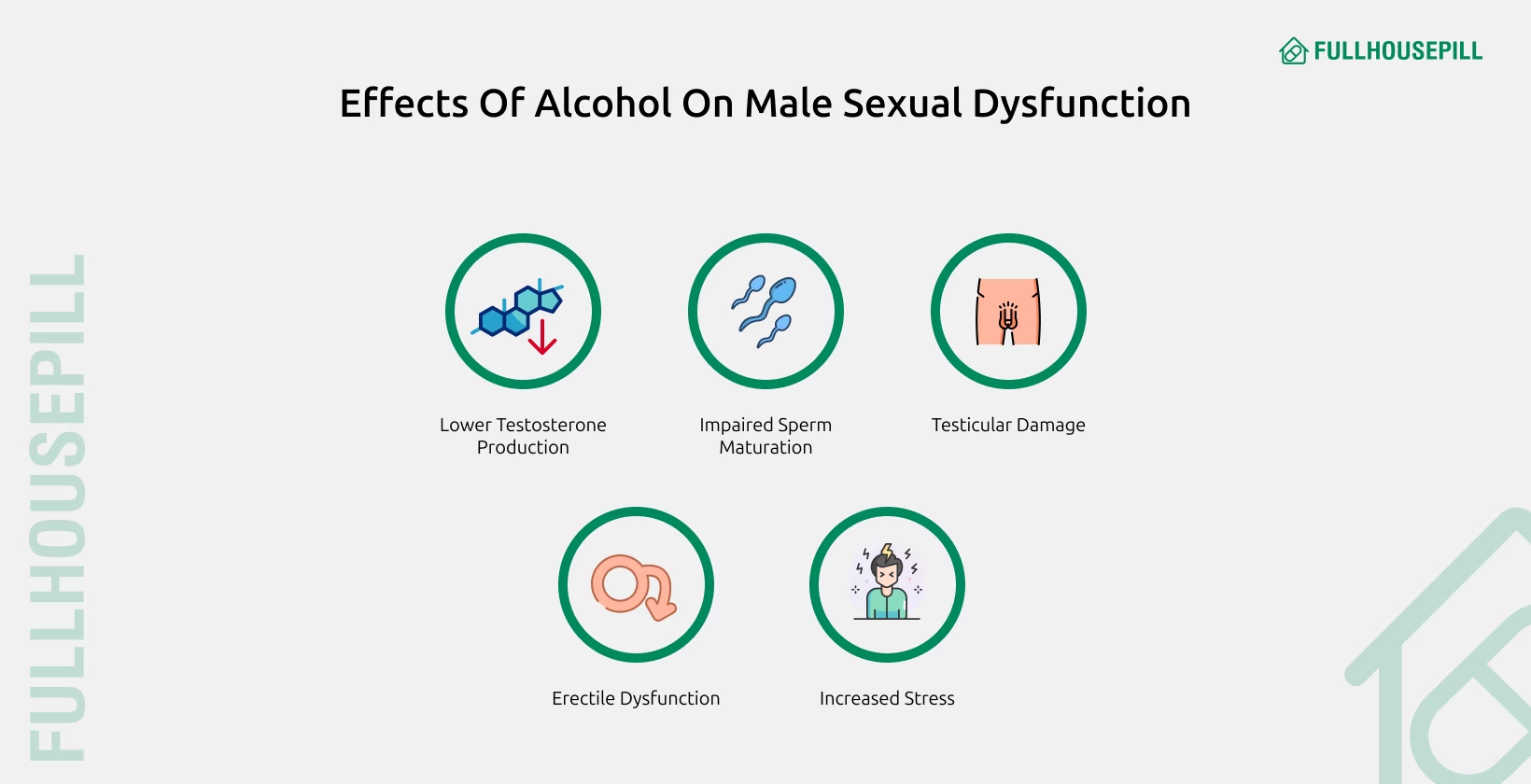
Yes, alcohol can negatively affect male sexual function, especially when used heavily or over long periods. Short-term alcohol use may reduce inhibitions and increase sexual confidence, but high doses impair erection, ejaculation, and overall performance. Alcohol acts as a central nervous system depressant. It slows nerve signals that coordinate arousal and delays the release of hormones involved in sexual response. Chronic alcohol use damages the liver, reduces testosterone production, and leads to neuropathy. These changes disrupt the vascular and hormonal systems necessary for erections and desire. Men with alcohol dependence often report reduced libido, weak or short-lived erections, and difficulty achieving orgasm. Alcohol also increases the risk of developing conditions like liver cirrhosis, hypertension, and depression, each of which independently contributes to sexual dysfunction. In many men, excessive drinking masks underlying sexual disorders and worsens them over time.
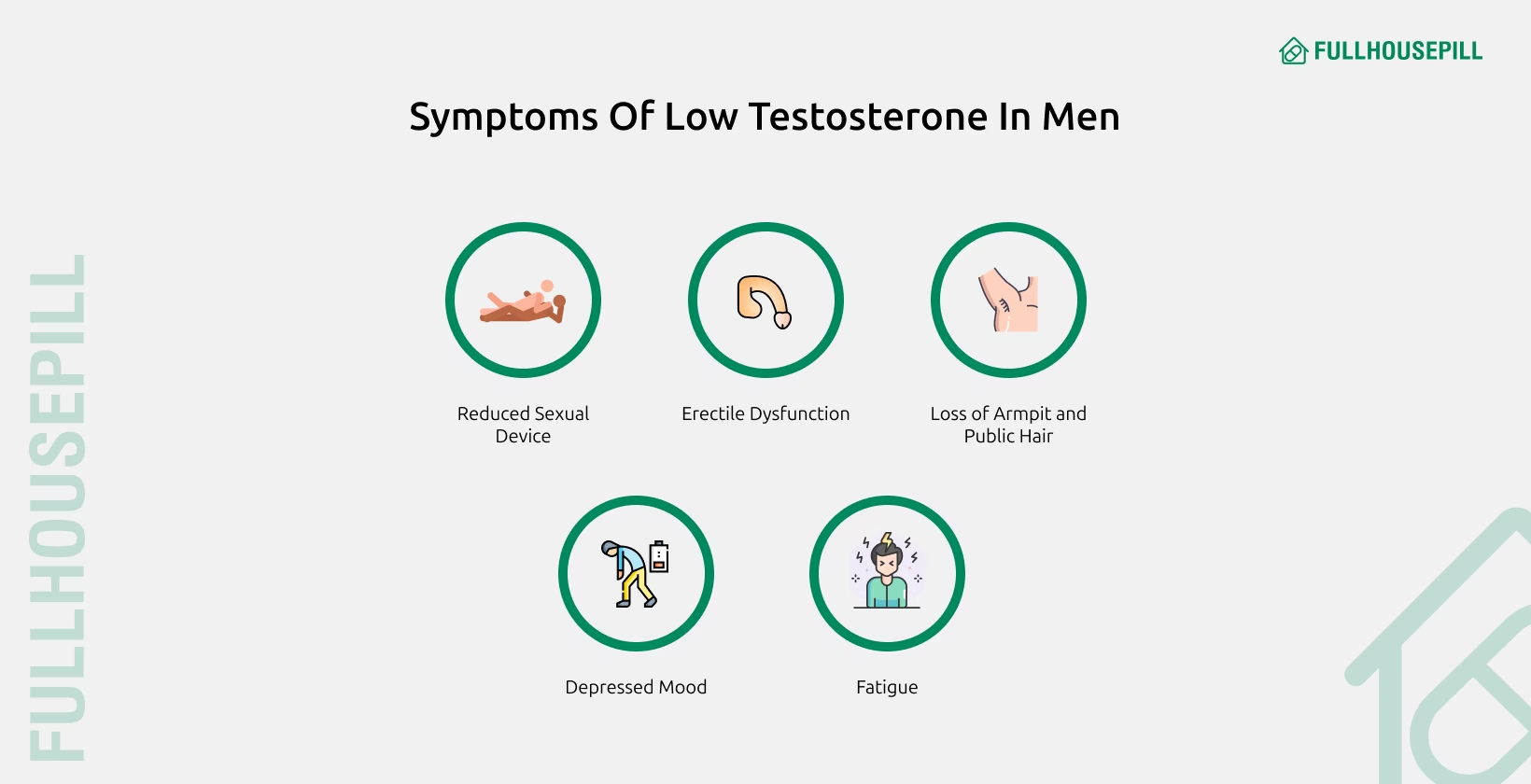
Yes, low testosterone is a major hormonal cause of male sexual dysfunction. Testosterone supports libido, spontaneous erections, and sexual energy. When levels drop below the normal range, men often report reduced sexual interest, fewer erotic thoughts, and lower response to stimulation. Clinical hypogonadism is typically diagnosed when testosterone levels fall below 300 ng/dL, combined with symptoms such as fatigue, depression, or decreased morning erections. Testosterone levels decline gradually with age but may also drop due to obesity, diabetes, injury, or chronic illness. In men with low testosterone, sexual dysfunction may include both decreased desire and mild-to-moderate erectile issues. These problems often improve with testosterone replacement therapy if no other underlying cause is present. However, not all sexual issues are caused by testosterone. A full medical evaluation is needed to rule out vascular, neurological, or psychological causes before starting hormone therapy.
DSM-5 criteria provide a structured, symptom-based framework for diagnosing male sexual dysfunction. The diagnosis requires symptoms to be persistent, distressing, and not caused by other health or psychological conditions. Each subtype, erectile disorder, premature ejaculation, delayed ejaculation, or low sexual desire, has specific diagnostic markers. Use the table below to understand how DSM-5 classifies and evaluates each type:
| Category | DSM-5 Diagnostic Criteria |
|---|---|
| General Requirements | Symptoms present for ≥6 months, occur in 75–100% of sexual activity, cause significant distress, and are not better explained by other factors |
| Erectile Disorder | Difficulty achieving or maintaining an erection or reduced erectile rigidity during activity |
| Premature Ejaculation | Ejaculation within 1 minute of penetration, occurring before the person desires |
| Delayed Ejaculation | Marked delay, infrequency, or absence of ejaculation despite adequate stimulation |
| Male Hypoactive Sexual Desire | Persistent low or absent sexual interest or desire |
| Assessment Tools | Clinical interview, physical exam, and psychological screening to rule out contributing factors |
Erectile Dysfunction (ED) is treatable through medications, mechanical devices, lifestyle changes, and psychological therapies. The right ED treatment depends on the cause, severity, patient preference, and response to earlier interventions. While medications are the most commonly used first-line therapy, non-pharmacological options can be highly effective, especially for men with complex or multifactorial ED.
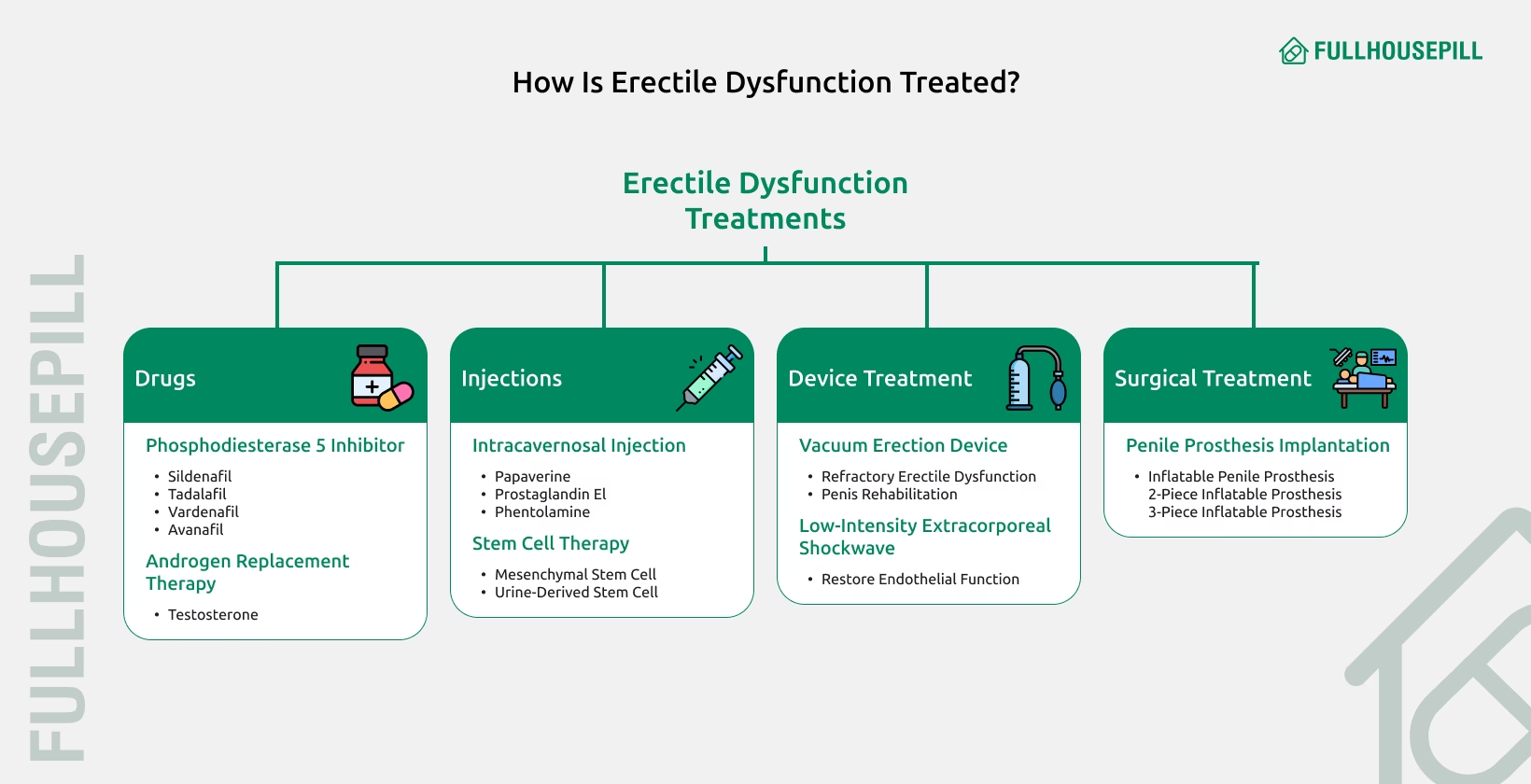
Pharmaceutical treatments, especially PDE5 inhibitors, are the first-line option for most men with ED. They work by increasing blood flow to the penis, supporting an erection during sexual arousal.
| Medication | Brand Name | Typical Dose | Onset Time | Duration |
|---|---|---|---|---|
| Sildenafil | Viagra | 50mg | 30-60 minutes | 4-6 hours |
| Tadalafil | Cialis | 10mg | 30 minutes | 24-36 hours |
| Vardenafil | Levitra | 10mg | 60 minutes | 5-7 hours |
| Avanafil | Stendra | 50-100mg | 30-45 minutes | 4-6 hours |
Below is a list of phosphodiesterase type 5 (PDE5) inhibitors that help treat erectile dysfunction.
Tadalafil is often preferred for its long-lasting action, while vardenafil is associated with fewer side effects.
Eroxon represents a significant advancement as the first over-the-counter topical treatment for ED approved by the FDA. This gel contains ethanol, glycerine, and carbomer, and works by evaporating and cooling the skin before gradually becoming warm, stimulating nerve endings to release nitric oxide. Clinical trials showed that 65% of men achieved an erection within 10 minutes compared to 30-60 minutes for oral medications.
Intracavernosal injections are highly effective treatments that work by relaxing smooth muscle in blood vessel walls, causing them to dilate and fill the penis with blood. The main injectable medications include:
Injectable therapies trigger spontaneous erections without sexual stimulation, with erections typically developing in 10-15 minutes and lasting 30-60 minutes. These medications are particularly useful for men with severe ED or those who don’t respond to oral medications.
MUSE (Medicated Urethral System for Erection) is an FDA-approved urethral suppository containing alprostadil. The medication is inserted into the urethra using a special applicator and is available in doses of 125, 250, 500, and 1000 micrograms. MUSE begins creating an erection in about 5-10 minutes, with sexual activity recommended within 10-30 minutes of administration.
Testosterone replacement therapy (TRT) can be beneficial for men with ED who also have low testosterone levels. Research indicates that testosterone replacement monotherapy can improve erectile function in men with mild ED, but not moderate and severe ED. TRT is particularly effective when combined with PDE5 inhibitors in men who are unresponsive to PDE5 inhibitors alone.
Vacuum erection devices are non-invasive mechanical aids that create an erection by drawing blood into the penis using negative pressure. A VED consists of:
Studies show that vacuum devices are effective in producing erections in 89% of men. Long-term research indicates that patient and partner satisfaction rates are 82-87% with regular use reported by 69-70% of patients. However, the dropout rate is approximately 19-33% within the first year, primarily due to insufficient erections, partner refusal, or discomfort.
Penile implants are surgical devices that can restore erectile function when other treatments fail. There are two main types:
Patient satisfaction rates are typically high, with studies showing that most patients and partners report satisfaction with penile implants. The surgery typically takes 1-2 hours and is performed as outpatient surgery.
Newer mechanical devices include external penile support systems like the “Erektor” device, which consists of two rings attached to a rigid rod that provides length and rigidity to the penile shaft during intercourse. While these devices show promise, more research is needed to establish their efficacy.
Lifestyle modifications can significantly improve erectile function and are often recommended as first-line interventions. Key changes include:
Research shows that these lifestyle interventions can be as powerful as medications in improving erectile function.
Controlling diabetes is crucial, as ED is three times more common in diabetic men (28% vs 9.6%). Risk factors for ED in diabetic men include:
Psychological treatment is essential when mental health or emotional factors contribute to ED. The four main goals of psychotherapy for ED include:
Studies demonstrate that psychotherapy combined with medical treatment significantly increases the effectiveness of ED interventions. For men with stress-related ED, having the partner involved in therapy resolves the problem 50-70% of the time.
Low-intensity shockwave therapy (LI-ESWT) is a non-invasive treatment that uses targeted sound waves to stimulate penile tissue and encourage blood flow. Research shows that shockwave therapy can provide mild to moderate improvement in patients with ED of varying etiologies.
A 2019 meta-analysis found that patients receiving shockwave therapy were 8.5 times more likely to achieve a clinically meaningful improvement compared to control groups. However, it’s important to note that shockwave therapy is not yet FDA-approved for ED and should only be performed in clinical research settings.
Platelet-rich plasma therapy involves injecting concentrated platelets from the patient’s own blood into the penis. PRP contains growth factors that may help regenerate blood vessels and improve erectile function. However, studies have shown little to no benefit from PRP in treating ED, and more research is needed to establish its efficacy.
Stem cell therapy involves using stem cells to renew and repair damaged penile tissue. While promising in animal studies, success in humans has been inconsistent and largely dependent on the stem cell donor. This treatment remains investigational.
Gene therapy represents a novel approach that would deliver genes to produce proteins that may not be functioning properly in penile tissue. While experimental models show promise, human studies are limited, and regulatory approval may take considerable time.
The best pills for ED are prescription medications like sildenafil, tadalafil, vardenafil, and avanafil. Each of these medications varies in onset, duration, and side effect profile. These drugs belong to the class of PDE5 inhibitors. They are clinically proven to improve erectile function in men with mild to severe ED. Below is a table for comparing the best pills for ED based on timing, use cases, and personal preferences. Always recommend a doctor’s consultation before use.
| Medication Name | Generic Name | Onset Time | Duration | Best For | Notes |
|---|---|---|---|---|---|
| Viagra | Sildenafil | 30-60 minutes | Up to 4 hrs | On-demand use | Most prescribed ED pill |
| Cialis | Tadalafil | 30-45 minutes | Up to 36 hrs | Long-lasting effect or daily use | Can be taken as a low-dose daily pill |
| Levitra | Vardenafil | 30-60 minutes | 4–5 hrs | Men with diabetes | Similar to sildenafil |
| Stendra | Avanafil | 15-30 minutes | 6 hrs | Fast-acting use | Fewer side effects in some users |
| Cenforce | Sildenafil (Generic) | 30-60 minutes | Up to 4 hrs | Affordable option | Same active ingredient as Viagra |
| Vidalista | Tadalafil (Generic) | 30-45 minutes | Up to 36 hrs | Budget-friendly long-duration pill | Same active ingredient as Cialis |
Men seeking the best pills for ED should consult a healthcare provider to match the right medication with their health status, lifestyle, and expectations. Factors like onset time, duration of action, side effects, and interaction with other medications should be evaluated before starting treatment.
Replace the list with “Behavioral Techniques, Pelvic-Floor Rehabilitation, Counseling and CBT, Partnered Education, Prescription Medication For PE”
PE treatment includes behavioral therapy, pelvic-floor rehabilitation, psychological interventions, and medications.
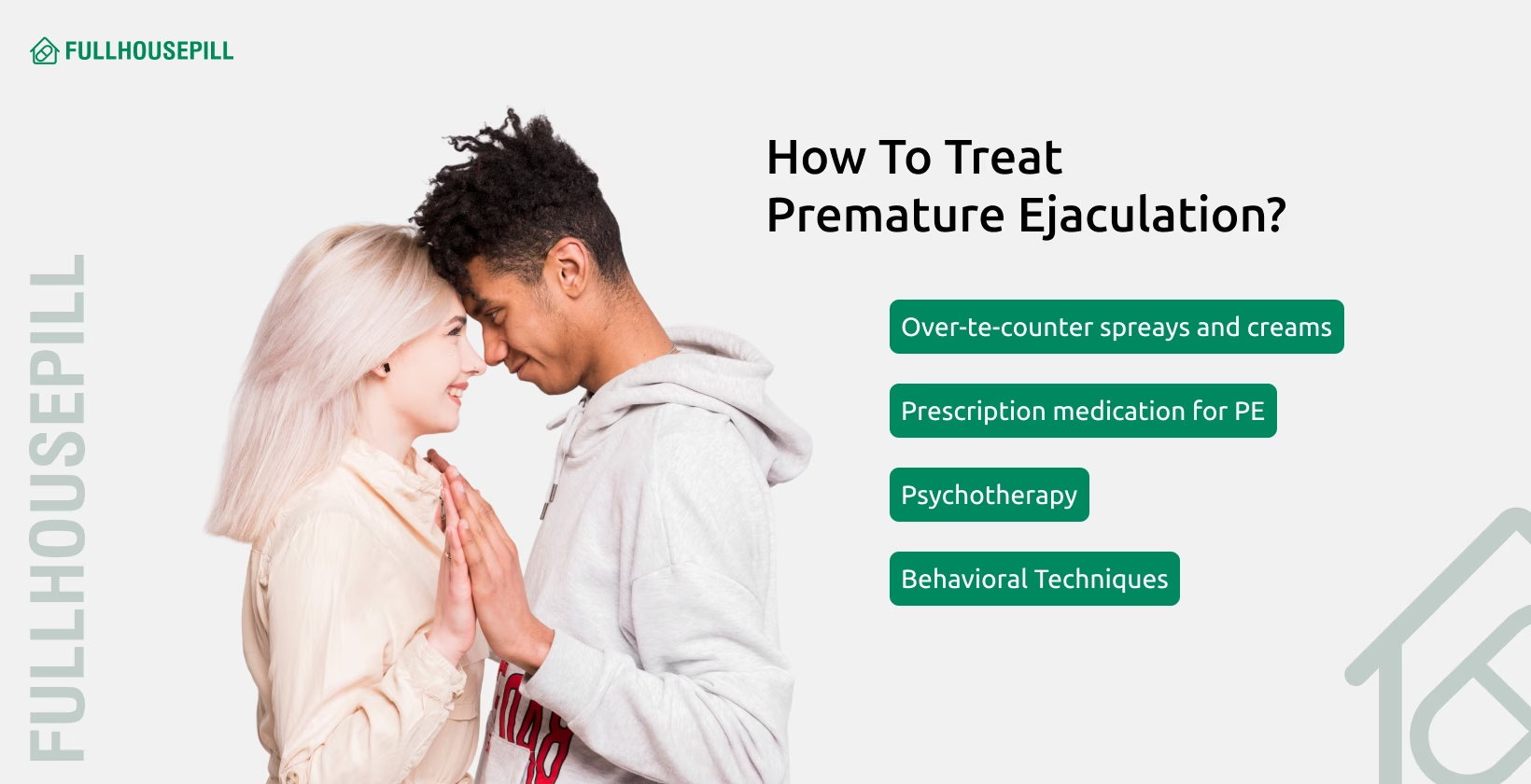
Behavioral techniques are physical interventions that reduce arousal to delay ejaculation. These include Stop-start, squeeze, and precoital masturbation techniques. Stop-start technique involves repeated sexual stimulation followed by short pauses before ejaculation. Squeeze technique includes applying pressure to the penis tip until the urge to ejaculate subsides. Precoital masturbation lowers baseline arousal, often prolonging intravaginal ejaculation latency time (IELT) during intercourse. These methods are first-line for lifelong PE and are most effective with consistent practice and partner support.
Pelvic-floor rehabilitation is a muscle-training program designed to improve control over the ejaculatory reflex. It involves performing Kegel exercises that target the bulbocavernosus and pubococcygeus muscles, which contract during ejaculation. Stronger pelvic muscles delay reflex activity and improve voluntary control. A study found that after 12 weeks of training, 82% of participants increased their IELT from under 1 minute to over 2.4 minutes.
CBT is a structured psychological treatment that identifies and changes unhelpful thoughts and behaviors. In PE, CBT helps reduce performance anxiety, low self-confidence, and fear of failure, all of which can trigger rapid ejaculation. It retrains negative thinking patterns and builds emotional regulation. CBT is most effective in men with acquired PE due to psychological or relational issues. When combined with sex education, it significantly improves long-term outcomes.
Partnered education involves teaching both partners about PE and its management strategies. It promotes open communication, reduces stigma, and encourages mutual participation in behavioral training. Couples who learn and apply techniques together are more likely to see improvement in ejaculatory control and overall relationship satisfaction. It also enhances adherence to therapeutic routines.
PE medications include oral drugs and topical agents that delay ejaculation by altering neural or sensory pathways. Dapoxetine, a short-acting SSRI, delays ejaculation by increasing serotonin activity in the brain. Off-label SSRIs like paroxetine or sertraline, taken daily, extend IELT by modulating central serotonin levels. Topical anesthetics such as lidocaine-prilocaine reduce penile sensitivity by numbing the skin. These options are ideal when non-pharmacological approaches are insufficient or when PE has a strong neurochemical basis.
Low libido in men is treated through counseling, hormone therapy, and off-label medications depending on the underlying cause. Doctors first determine whether the low sexual desire is chronic (lifelong/generalized) or acquired (generalized or situational). Treatment goals focus either on restoring libido or helping the individual and couple adapt if reversal is unlikely.
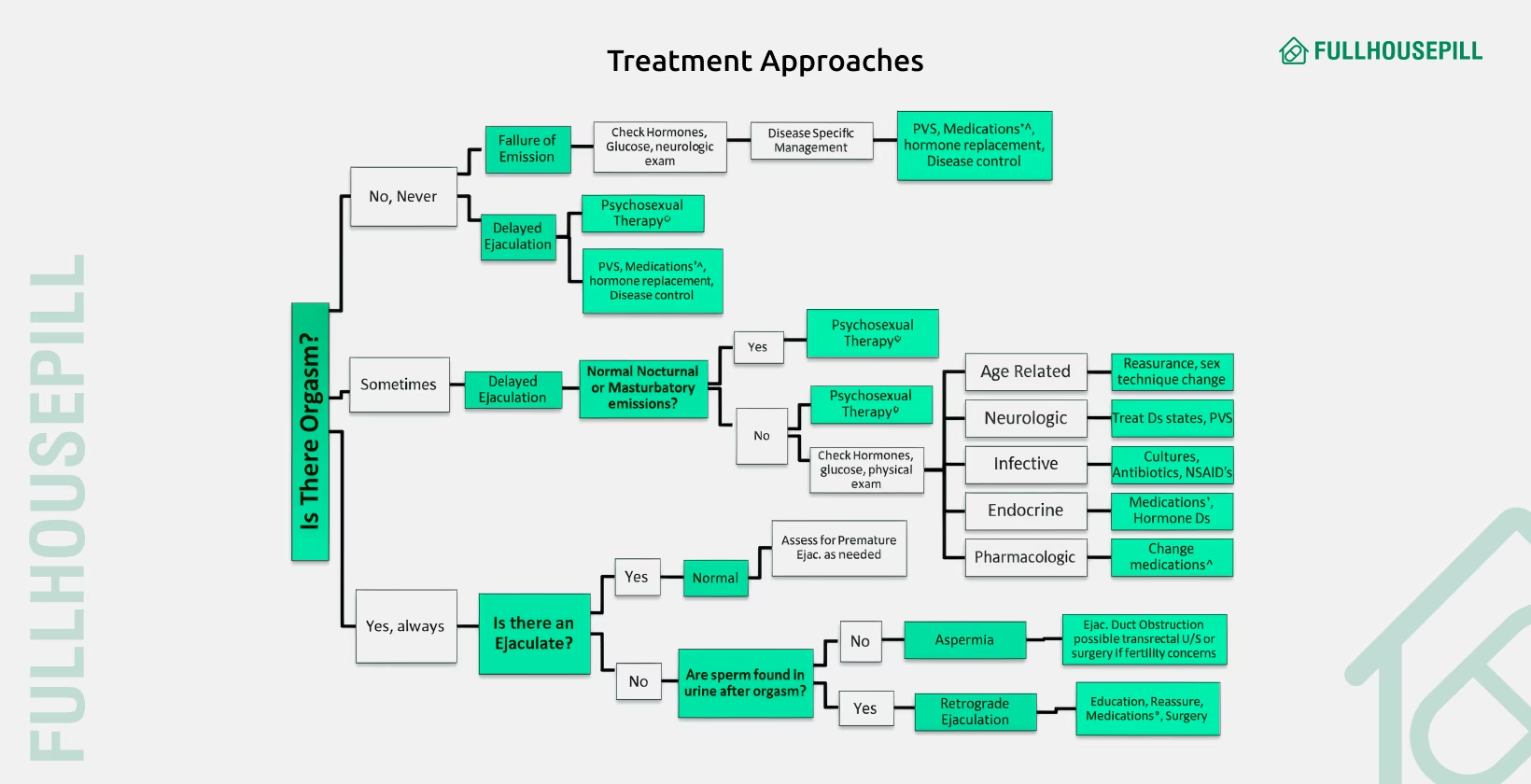
Delayed ejaculation or anorgasmia in men is treated using sex therapy, behavioral retraining, and off-label medications based on cause and severity. Doctors begin by identifying whether the condition is lifelong or acquired. Lifelong (primary) delayed ejaculation (DE) often lacks clear biological causes, while acquired cases may stem from psychological factors, medication use, or neurological issues. When caused by medication or illness, the underlying issue must be resolved first.
Men experiencing SSRI-induced anorgasmia may benefit from medications like amantadine, cyproheptadine, buspirone, bupropion, or nefazodone. Reducing SSRI dosage can also help. Some clinicians use yohimbine, a plant-derived compound, which has shown success in treating orgasmic dysfunction in small studies. Treatment selection depends on the individual’s history, cause of dysfunction, and response to therapy.
Natural remedies for sexual dysfunction in men include lifestyle modifications, herbal supplements, and alternative therapies that support vascular health, reduce stress, and enhance sexual function. Men can benefit from these interventions especially when dysfunction is caused by poor circulation, psychological stress, or hormonal imbalance. Natural strategies may not work for all cases, especially where a medical condition like diabetes or neurological damage is involved.
| Remedy Type | Examples | Function |
|---|---|---|
| Lifestyle Changes | Healthy diet, regular exercise, stress reduction, weight loss | Improves vascular health, reduces risk factors |
| Herbal Supplements | Ginseng, Ashwagandha, Maca, L-arginine | Enhances libido, improves nitric oxide availability |
| Alternative Therapies | Acupuncture, psychotherapy | Reduces anxiety, improves psychological ED |
| Avoidance Strategies | Quit smoking, limit alcohol | Reduces vascular and neurological damage |
| Pelvic Exercises | Kegel exercises | Strengthens muscles involved in erection and ejaculation |
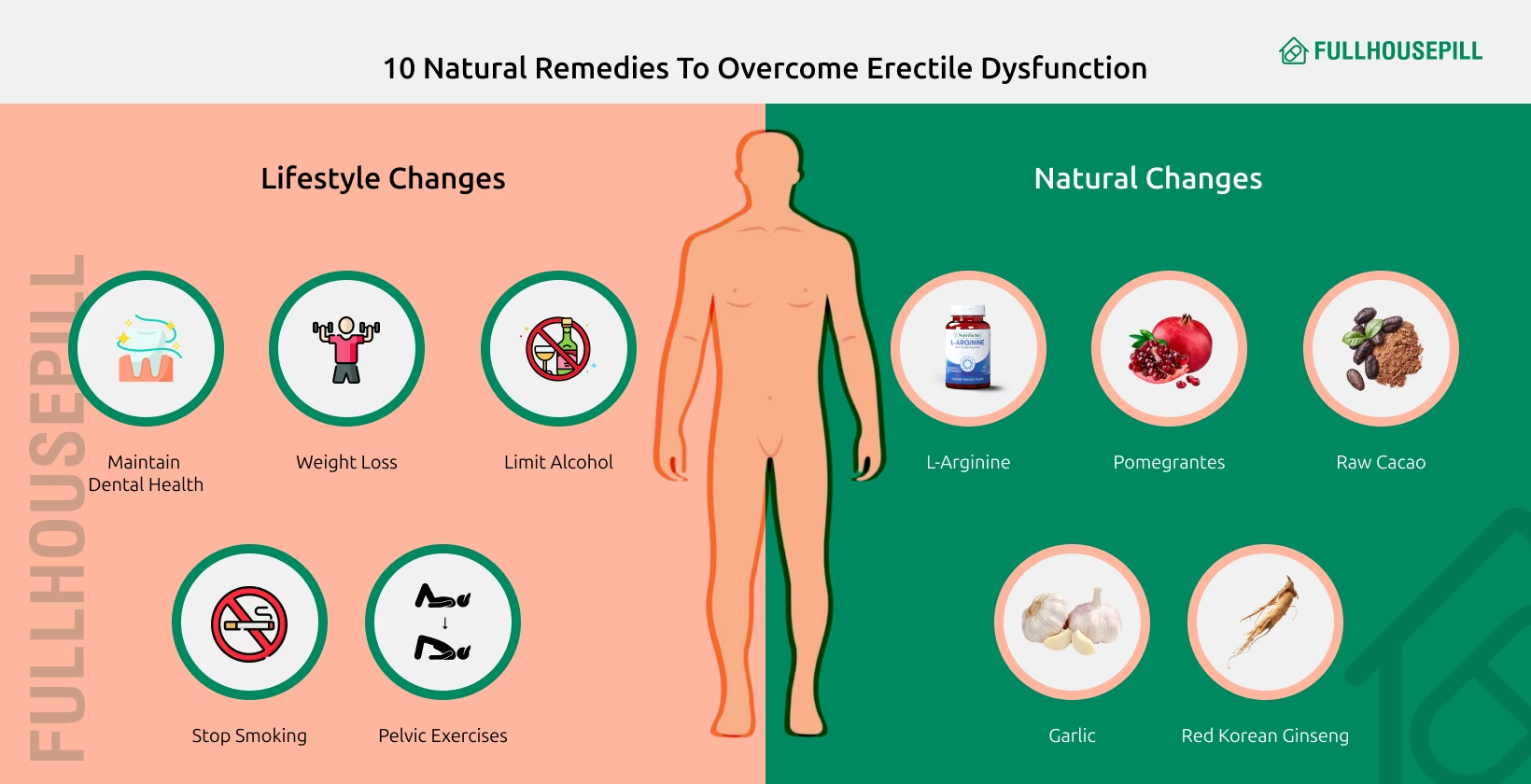
Men should consult a healthcare professional before starting natural remedies, especially if taking medications like antihypertensives or SSRIs. Scientific evidence for many herbal remedies is still evolving, and some may interact with prescription drugs or exacerbate health conditions. Natural therapies are best used as adjunct treatments or for mild cases. Persistent or severe sexual dysfunction may require evaluation and treatment with medically approved interventions.
Yes, food can help improve sexual dysfunction, especially erectile dysfunction, by supporting blood flow, hormone balance, and vascular health. A diet high in antioxidants, flavonoids, and healthy fats supports nitric oxide production, which is essential for achieving and maintaining erections. Below is a table for specific foods known to benefit sexual function.
| Food | Key Nutrient | Effect on ED |
|---|---|---|
| Leafy greens | Nitrates | Improve blood flow by boosting nitric oxide |
| Beets | Nitrates | Enhance vasodilation and erection quality |
| Dark chocolate | Flavonoids | Increase nitric oxide and reduce blood pressure |
| Fatty fish | Omega-3 fatty acids | Improve cardiovascular health and hormone levels |
| Nuts and seeds | L-arginine, zinc | Support testosterone and erection quality |
| Berries | Anthocyanins and flavonoids | Reduce risk of ED through antioxidant effects |
| Tomatoes | Lycopene | Improve prostate and vascular health |
| Oats | Avenanthramides | Support blood vessel dilation |
Incorporating food for erectile dysfunction into a daily routine can yield noticeable benefits, especially when combined with regular exercise and reduced alcohol or tobacco use. A diet based on whole grains, fresh produce, nuts, and lean proteins mirrors the Mediterranean diet, which has been clinically linked to lower ED risk in aging men.
Yes, certain vitamins for ED may support sexual health by improving blood flow, hormone regulation, and nitric oxide production. While they’re not a standalone cure, some nutrients play a supportive role in managing erectile dysfunction and boosting libido. For example, vitamin D plays a role in regulating vascular function and testosterone production. Low levels are commonly found in men with ED, and supplementation may help restore erectile response. B vitamins, particularly niacin (B3) and folate (B9), help facilitate blood vessel dilation by increasing nitric oxide availability, which is essential for maintaining erectile function. A 2020 systematic review of 11 randomized controlled trials found that niacin (vitamin B3) at 1500 mg daily significantly improved erectile function (p = 0.004), while vitamins A, C, and E showed no measurable benefit for sexual function in either men or women.Zinc supports testosterone synthesis and is especially helpful in men with deficiency-related ED. Similarly, the amino acid L-arginine contributes to nitric oxide production and has shown moderate benefit in improving penile blood flow when used in combination with pycnogenol or other vasodilators. Although vitamins for ED may help, results vary by individual. They should not replace medical evaluation or prescription treatments like PDE5 inhibitors. Always consult a healthcare provider to assess the cause of sexual dysfunction and ensure safe, targeted use of supplements.
Sexual dysfunction can lead to emotional distress, communication breakdown, and reduced intimacy in relationships. Men experiencing issues like erectile dysfunction, premature ejaculation, or low libido often feel shame, guilt, or frustration. These emotional responses can create distance from their partners, lower self-esteem, and cause performance anxiety. Over time, unresolved dysfunction may result in conflict, avoidance of sexual activity, or relationship dissatisfaction. Partners may interpret sexual withdrawal as rejection, even when the cause is physical or psychological. This miscommunication can fuel resentment, mistrust, or infidelity in some cases. Addressing sexual dysfunction early, through honest communication, counseling, or medical treatment, can strengthen the emotional bond and restore sexual satisfaction in a relationship.
You should see a doctor for sexual dysfunction if it is persistent, worsening, or affecting your mental health or relationship quality. Men should consult a healthcare provider when:
Doctors can evaluate whether the dysfunction is caused by hormonal imbalance, cardiovascular disease, medication side effects, or psychological stress. Early diagnosis helps prevent complications and offers more treatment options, from lifestyle changes and medications to sex therapy. Untreated sexual dysfunction can worsen over time, especially when linked to progressive conditions like peripheral artery disease or testosterone deficiency.
Over-the-counter (OTC) ED pills are increasingly popular among men looking for alternatives to prescription medications like Viagra. While prescription drugs […]
Cialis, also known as tadalafil, is a PDE5 inhibitor widely used for male enhancement and treatment of erectile dysfunction. Understanding
Sildenafil or Viagra is a medication that helps men improve their sexual performance. It supports firmer and longer-lasting erections. It
Impotence or Erectile Dysfunction (ED) is the persistent inability to maintain a penile erection long enough for satisfactory sexual activity.
A Rhino pill is a sexual enhancement pill often marketed as an easy solution for men to improve erections. It
Erectile dysfunction (ED), also called male impotence, is the inability to get or maintain an erection for sexual activity. This
Testosterone plays a central role in erectile function through nerve support, nitric oxide regulation, and vascular smooth muscle health. Normal
Cialis is a popular Erectile Dysfunction (ED) drug and has some hypotensive effects (lowers blood pressure), though its clinical significance
The development of phosphodiesterase type 5 inhibitors like Sildenafil, Tadalafil, Vardenafil, and Avanafil established a pharmacological standard in the treatment
Vardenafil is a phosphodiesterase type 5 (PDE5) inhibitor prescribed for erectile dysfunction. It is sold under the brand names Levitra
Erectile dysfunction occurs due to vascular, neurogenic, hormonal, psychogenic, or drug-induced causes. Sometimes it is a side effect of the
Tadalafil is a PDE5 inhibitor approved for erectile dysfunction (ED), benign prostatic hyperplasia (BPH), and pulmonary arterial hypertension (PAH). It
Tadalafil, the active ingredient in Cialis, is a widely prescribed drug for erectile dysfunction, but its interaction with alcohol raises
Tadalafil is an FDA-approved medication for Erectile Dysfunction. Its use has helped men achieve and maintain a strong erection during
Combining sildenafil (Viagra) with tadalafil (Cialis) is not advised. Both drugs work in the same way as PDE5 inhibitors. Some
Vardenafil and tadalafil differ in potency, duration, onset, dosing, and approved uses. Vardenafil demonstrates higher potency at the molecular level
Yes, pregnancy from precum (pre-ejaculate) is possible, although the risk is relatively low. Pre-ejaculate can contain sperm in some individuals,
When a woman takes sildenafil (Viagra), the drug increases blood flow to the genital area, potentially enhancing arousal, sensitivity, and
Sildenafil citrate, commonly prescribed for erectile dysfunction, is available in doses ranging from 25 mg to 100 mg, with 50
Sildenafil (Viagra) typically has a shelf life of 2 years, but improper storage can reduce safety and efficacy through physical